Welcome to PICU Doc On Call, A Podcast Dedicated to Current and Aspiring Intensivists.
I’m Pradip Kama and I’m Rahul Damania, a third-year PICU fellow. I’m Kate Phelps, a second-year PICU fellow and we are all coming to you from Children’s Healthcare of Atlanta, Emory University School of Medicine, joining Pradip and Rahul today. Welcome to our episode, where will be discussing rhabdomyolysis and associated acute kidney injury in the ICU.
Rahul: Here’s the case, a 7-year-old female presents to the ED with three days of fever, poor PO, and diffuse myalgia. In the ED, her vital signs are T 39.1C, HR 139, BP 82/44, RR 32. She is pale and diaphoretic, complaining weakly about how much her legs hurt. Her parents note that she has not been peeing very well since yesterday, and when she does pee it is “very concentrated, almost brown.” She’s also been spending all her time on the couch and has asked to be carried to the bathroom when she does need to go.
An IV is placed by the emergency room team, and she is given a fluid bolus, acetaminophen, and initial labs are drawn (CMP, CBC, RSV/Flu swab) before she is admitted to the PICU. In the PICU, her fever is better and her vitals have improved to T 37.7, HR 119, BP 115/70, and RR 25. Her respiratory swab has just resulted positive for Influenza A. Further labs are sent, including creatine kinase (CK), coagulation studies, and a urinalysis. Labs are notable for K 3.9, Bicarb 22, BUN 15, Cr 0.8, and CK 5768 IU/L. Her urinalysis is notable for 1 WBC, 2 RBC, +3 blood, negative nitrites, and leukocyte esterase.
Kate: To summarize key elements from this case, this patient has:
- Influenza A, as evidenced by her respiratory swab, as well as her clinical prodrome.
- She has diffuse myalgias, as well as fevers, diaphoresis, and hypotension.
- Labs are most notable for elevated creatinine and elevated creatine kinase, as well as an abnormal urinalysis.
- All of which brings up a concern for rhabdomyolysis and myoglobin-induced acute kidney injury.
Before we get into this episode — let’s create a mental framework for this episode — we will dissect our case by highlighting key H&P components, visit a differential diagnosis, pivot to speaking about pathophysiology, and finally, speak about management!
- Rahul: Let’s transition into some history and physical exam components of this case.
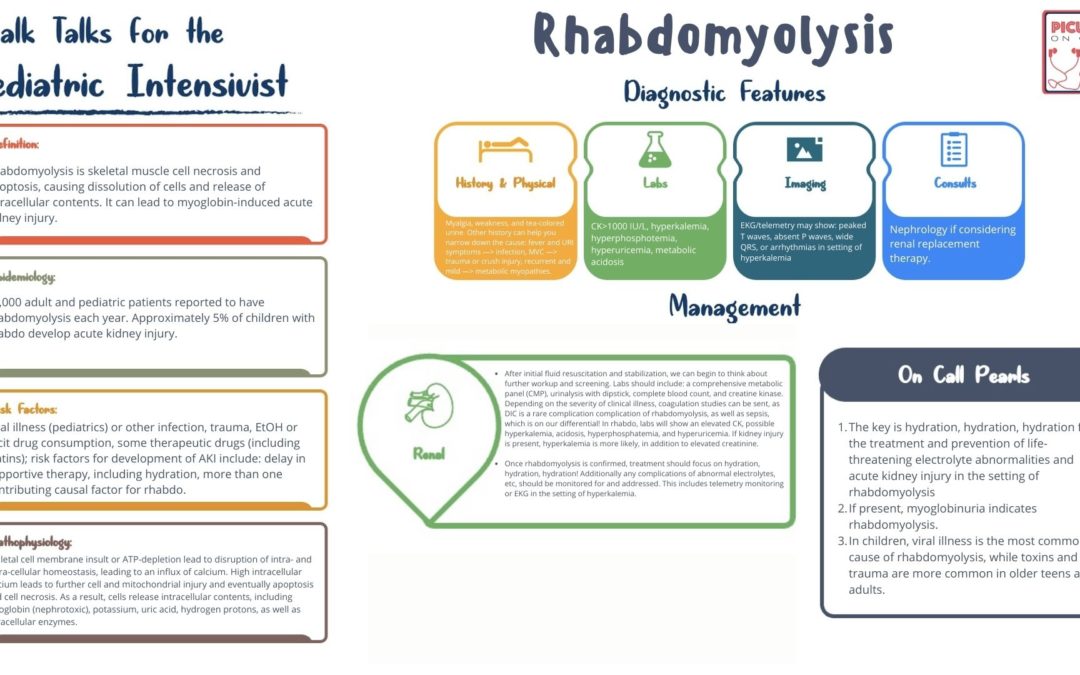
- The classic presentation of rhabdomyolysis is myalgias, muscle weakness, and tea-colored urine, all of which our patient has. Decreased urinary output can also accompany, a variety of reasons, but most notably if the patient has myoglobin-induced acute kidney injury. In our patient, poor PO is also probably contributing to her decrease in urine output. Red flag signs or symptoms will include anuria, hypotension, and altered mental status (which is rare but may indicate severe acidemia and deterioration)
- Pradip: As we think about our case, what other disease processes might be in our differential? As we dive in a bit more, we’ll come up with ways to distinguish between rhabdo and other things!
- Viral myositis – inflammation in the muscles in the setting of a viral illness, which can definitely happen with influenza and other common viruses
- Some other things which may cause reddish-brown urine, including hematuria, hemoglobinuria, porphyria, some specific foods or drugs (like rifampin, beets, food coloring — even ibuprofen)
- We also have to investigate a bit more to convince ourselves that our patient’s AKI is due to rhabdomyolysis, as it could be from dehydration, sepsis, NSAIDS, etc.
Kate: Let’s dive further into rhabdomyolysis!
Rhabdomyolysis affects over 25,000 adults and children every year. While toxins (including prescription drugs, alcohol, and illicit drugs) and trauma are two common causes of rhabdo in adults (and teens), infections, especially viruses, are the most common cause in young children. Influenza, EBV, and CMV are three most commonly reported.
What’s the pathophysiology of Rhabdomyolysis?
Rhabdomyolysis is the injury of skeletal muscle, which leads to cellular damage, apoptosis, and necrosis. As a result, skeletal muscle cells lyse and release their intracellular contents. Insult directly to the cell membrane and ATP-depletion are two mechanisms that can start the chain reaction leading to this cell death.
When the cell membrane itself is injured (as may happen in trauma or crush injury, metabolic conditions, or toxins), ionized calcium can freely enter the cell, leading to activation of proteases and phospholipases, which further injure the cell membrane, as well as mitochondria. As a result, the cell undergoes apoptosis and necrosis. When there is an ATP-depletion, pumps on the cell membrane important for maintaining sodium and calcium homeostasis between the intracellular and extracellular components become compromised. Intracellular calcium levels build, and the same process of cell and mitochondrial injury leads to apoptosis and necrosis.
To summarize, Rhabdomyolysis is an index example of cell adaptations, injury, and death. The key here is cell membrane damage which leads to downstream apoptosis.
Absolutely Rahul, the danger of this is that other intracellular contents are released into the extracellular space, including myoglobin, potassium, uric acid, intracellular enzymes, and many other things. Creatine kinase, or CK, released from cells is relatively indicative of rhabdo. Though no consensus criteria for rhabdo exist, most experts agree that serum CK level >1000 IU/L combined with the history and physical findings we will discuss is consistent with rhabdomyolysis.
This is especially important as there is are a multitude of pathologies that can cause a mild, transient increase in CK levels usually < 1000.
Pradip: One of the most common and most dangerous complications of rhabdomyolysis is acute kidney injury. While more common in adults, AKI occurs in ~5% of children with rhabdomyolysis. Let’s take a brief moment to discuss rhabdomyolysis-induced, or more specifically myoglobin-induced, acute kidney injury. While the mechanisms for myoglobin injury to the nephron aren’t entirely clear, most experts believe one of three things or, more likely, a combination of three things occur. Rahul, can you walk us through those?
Rahul: Sure, I’d love to!
- First, myoglobin is directly nephrotoxic, though notably only in an acidic environment!
- Second, it causes oxidation of ferrous oxide, leading to free radicals and reactive oxygen species, unregulated by usual intracellular processes.
- Third, myoglobin, through protein-binding, can precipitate in the tubule, leading to obstructive nephropathy.
Kate: Whew! That is a lot! Let’s take a break and review what we just learned:
Rhabdomyolysis is the injury of skeletal muscle leading to calcium influx into cells, which cascades into eventual apoptosis and necrosis. This leads to a massive release of intracellular components that upsets the overall homeostasis of the intra- and extracellular spaces. Myoglobin released from cells can directly injure the kidneys, leading to AKI. Potassium and hydrogen proton leakage, combined with AKI, can lead to life-threatening hyperkalemia and acidosis. CK is a serum measurement that can help confirm the diagnosis of rhabdomyolysis.
Rahul: Fun Fact Myoglobinuria usually only occurs in rhabdomyolysis (BUT not all rhabdomyolysis has myoglobinuria as it only spills out in urine above certain serum concentrations). Myoglobinuria can be inferred from a urine dipstick when there is moderate or large blood but few or no red blood cells. This is because the dipstick test for blood is non-specific for hemoglobin vs myoglobin! Myoglobin is also the reason the urine turns reddish-brown or “tea-colored.”
Pradip: Let’s change gears and talk about management. Kate, can you tell us about the management of rhabdomyolysis?
- Kate: With this patient, our first step should be resuscitation — always ABCs first! After initial fluid resuscitation and stabilization, we can begin to think about further workup and screening. Labs should include a comprehensive metabolic panel (CMP), urinalysis with dipstick, complete blood count, and creatine kinase. Depending on the severity of clinical illness, coagulation studies can be sent, as DIC is a rare complication of rhabdomyolysis, as well as sepsis, which is on our differential! In rhabdo, labs will show an elevated CK, possible hyperkalemia, acidosis, hyperphosphatemia, and hyperuricemia. If kidney injury is present, hyperkalemia is more likely, in addition to elevated creatinine.
- Once rhabdomyolysis is confirmed, treatment should focus on hydration, hydration, hydration! Additionally any complications of abnormal electrolytes, etc, should be monitored for and addressed. This includes telemetry monitoring or EKG in the setting of hyperkalemia.
Rahul: Remember, symptomatic hyperkalemia as evidenced by EKG changes, including wide QRS, absent P waves, or arrhythmias, including ventricular fibrillation, should be treated immediately. IV calcium administration will stabilize the cardiac membrane. Bicarbonate, insulin + glucose, and albuterol can quickly but only temporarily shift potassium into cells. Kayexalate and diuretics can remove potassium from the body.
- Pradip: Hydration is the most important treatment in rhabdomyolysis. There is a paucity of data, but most expert consensus suggests targeting a urine output of 3-4 ml/kg/hr while administering 2x maintenance fluids for children with rhabdo. Which fluid is the right fluid is still an area for more research, as studies have shown conflicting data about the benefits of NS vs LR vs bicarb-fluids. Normal saline without potassium can be used. Bicarbonate-containing fluids can be considered to buffer the urine on a case-by-case basis.
- Kate: And treatment of AKI should include avoidance of nephrotoxic medications and treatment of the underlying etiology. Renal replacement therapy should be considered for refractory fluid overload in the setting of oliguria or anuria, refractory acidosis (with pH<7.1), and refractory or life-threatening hyperkalemia. Remember those AEIOU reasons for RRT!
- With the resolution of the underlying cause, CK should peak in 3-5 days and then start to down-trend. Patients can be considered safe for discharge with the return of kidney function, normalization of electrolytes, and resolution of myoglobinuria.
We should note here that underlying metabolic myopathies can cause recurrent, mild rhabdomyolysis, though these children do not usually need critical care unless the cause for an exacerbation is sepsis or other potentially life-threatening illness!
- Kate: To wrap up, here are some take-away points:
- The key is hydration, hydration, hydration for the treatment and prevention of life-threatening electrolyte abnormalities and acute kidney injury in the setting of rhabdomyolysis
- If present, myoglobinuria indicates rhabdomyolysis.
- In children, viral illness is the most common cause of rhabdomyolysis, while toxins and trauma are more common in older teens and adults.
- Rahul: More information can be found
- “Rhabdomyolysis and acute kidney injury” from Bosch, et al, in the July 2009 issue of the New England Journal of Medicine and,
- “Pediatric rhabdomyolysis” in the June 2020 Pediatrics in Review
- References: (don’t read these)
- Szugye HS. Pediatric Rhabdomyolysis. Pediatr Rev. 2020 Jun;41(6):265-275. doi: 10.1542/pir.2018-0300. PMID: 32482689.
- Nance JR, Mammen AL. Diagnostic evaluation of rhabdomyolysis. Muscle Nerve. 2015 un;51(6):793-810. doi: 10.1002/mus.24606. Epub 2015 Mar 14. PMID: 25678154; PMCID: PMC4437836.
- Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009 Jul 2;361(1):62-72. doi: 10.1056/NEJMra0801327. Erratum in: N Engl J Med. 2011 May 19;364(20):1982. PMID: 19571284.
Pradip: This concludes our episode on rhabdomyolysis. We hope you found value in our short, case-based podcast. We welcome you to share your feedback, subscribe & place a review on our podcast! Please visit our website picudoconcall.org which showcases our episodes as well as our Doc on Call management cards. PICU Doc on Call is co-hosted by myself Dr. Pradip Kamat and Dr. Rahul Damania — with special guest Kate Phelps today. Stay tuned for our next episode! Thank you!