Today’s episode promises an insightful exploration into a unique case centered on retropharyngeal abscess in the PICU, offering a comprehensive analysis of its clinical manifestations, pathophysiology, diagnostic strategies, and evidence-based management approaches.
Today, we unravel the layers of a compelling case involving a 9-month-old with a retropharyngeal abscess, delving into the intricacies of its diagnosis, management, and the critical role played by PICU specialists. Join us as we navigate through the clinical landscape of RPA, providing not only a detailed analysis of the presented case but also valuable takeaways for professionals in the field and those aspiring to enter the world of pediatric intensive care. Welcome to PICU Doc On Call – where MED-ED meets the real challenges of the PICU.
Case Presentation
- Patient: 9-month-old male with rapid symptom onset, left neck swelling, fever, noisy breathing, and decreased oral intake.
- Initial presentation: Left neck swelling, limited neck mobility, and deteriorating condition.
- Imaging: Neck X-ray and CT scan with IV contrast confirmed Retropharyngeal Abscess (RPA).
- Management: High-flow nasal cannula, intravenous antibiotics, and consultation with ENT. PICU admission for comprehensive care.
Key Elements
- Rapid Symptom Onset
- Neck Swelling & Drooling
- Limited Neck Mobility
Problem Representation
- A previously healthy 9-month-old male with a recent upper respiratory infection, presenting with rapid-onset left neck swelling, fever, and respiratory distress. Imaging suggestive of a Retropharyngeal Abscess, requiring urgent PICU management for airway protection and antibiotic therapy.
Pathophysiology of RPA
- Anatomy of retropharyngeal space
- Rapid communication of infections via lymph nodes
- Infection sources: dental issues, trauma, localized infections (e.g., otitis, URI)
Dangers of RPA
- Airway compromise and posterior mediastinitis
- Progression from cellulitis to abscess
- Microbial suspects: Group A Streptococcus, anaerobes, Staphylococcus aureus, Haemophilus influenza, Klebsiella, Mycobacterium avium-intracellulare
Clinical Manifestations
- Seen predominantly in children aged 3-4 years
- Non-specific symptoms in the acute setting
- Pronounced symptoms in PICU: neck pain, stiffness, torticollis, muffled voice, stridor, respiratory distress
Diagnostic Workup
- Thorough history and physical examination
- CT scan with contrast as the gold standard
- Blood culture, CRP, and procalcitonin for infection severity
Clinical Pearls
- Limited neck mobility is the most specific physical exam finding
- Younger age and signs of airway obstruction indicate a complicated course
Management of RPA
- Antibiotic therapy: Up to 50% cases can be treated with IV antibiotics
- Surgical drainage may be needed if no improvement or persistent respiratory distress
- Duration of therapy: 10 to 14 days
- Controversial use of steroids for reducing airway swelling
Complications of RPA
- Upper airway obstruction, aspiration pneumonia, internal jugular thrombosis, carotid artery sheath rupture
- Mediastinitis: severe inflammation, infection of mediastinal tissues
Patient’s Clinical Course
- Respiratory viral panel: RSV, adenovirus, rhino/enterovirus
- Intubation due to worsening respiratory distress
- Incision and drainage (I&D) by ENT
- Cultures grew MRSA
- Extubation after air leak detection; discharged on oral Clindamycin
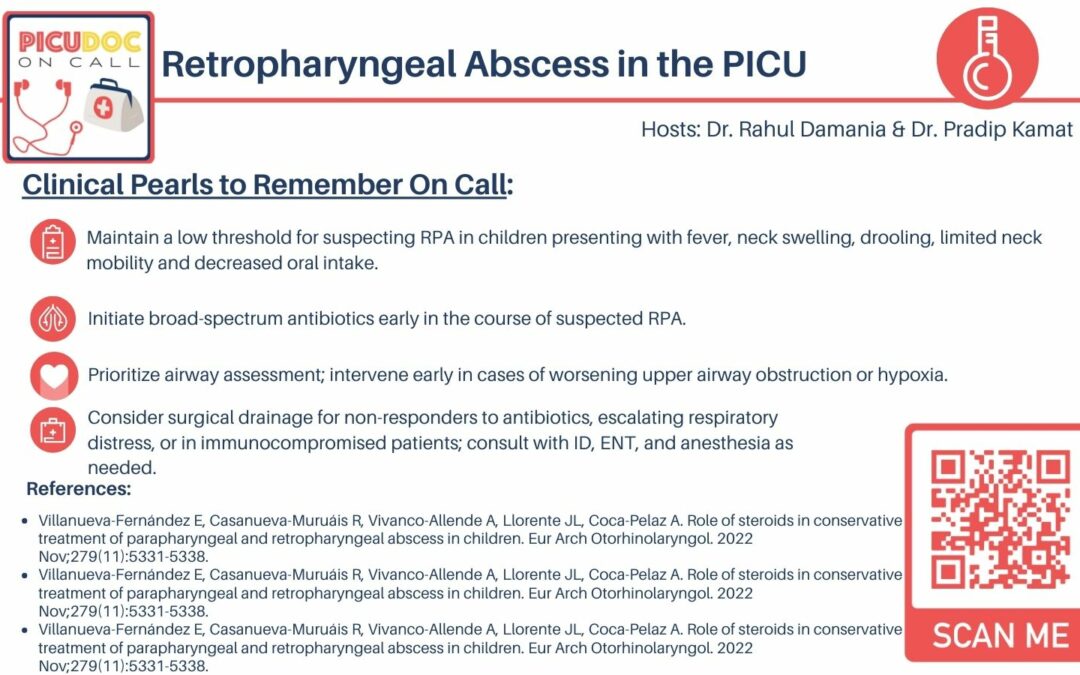
Clinical Takeaways
- Maintain a low threshold for suspecting RPA
- Initiate broad-spectrum antibiotics early
- Prioritize airway assessment and intervene early in cases of worsening upper airway obstruction or hypoxia
- Consider surgical drainage for non-responders, escalating respiratory distress, or immunocompromised patients
Conclusion
- Emphasize the critical nature of RPA in children and the importance of early intervention.
- Complications include upper airway obstruction, aspiration pneumonia, and potential vascular complications.
References
- Villanueva-Fernández E, et al. (2022) Role of steroids in conservative treatment of parapharyngeal and retropharyngeal abscess in children. Eur Arch Otorhinolaryngol.
- Akhavan M. (2021) Ear, Nose, Throat: Beyond Pharyngitis: Retropharyngeal Abscess, Peritonsillar Abscess, Epiglottitis, Bacterial Tracheitis, and Postoperative Tonsillectomy. Emerg Med Clin North Am.
- Reilly BK, Reilly JS. (2012) Retropharyngeal abscess: diagnosis and treatment update. Infect Disord Drug Targets.