Today’s case presentation involves a 2-year-old girl who was previously healthy and was admitted to the Pediatric Intensive Care Unit (PICU) for acute respiratory distress characterized by increased work of breathing and wheezing.
Case Presentation
A 2-year-old girl with acute respiratory distress due to RSV infection
- Presented with increased work of breathing, wheezing, and no fever
- Started on High Flow Nasal Cannula (HFNC) therapy in the PICU
Key Elements:
- Prodrome of URI symptoms
- Increased respiratory effort (nasal flaring, intercostal retractions, decreased lung base air entry)
- HFNC improved the work of breathing and oxygen saturation
Physiology of HFNC
Mechanisms of Action
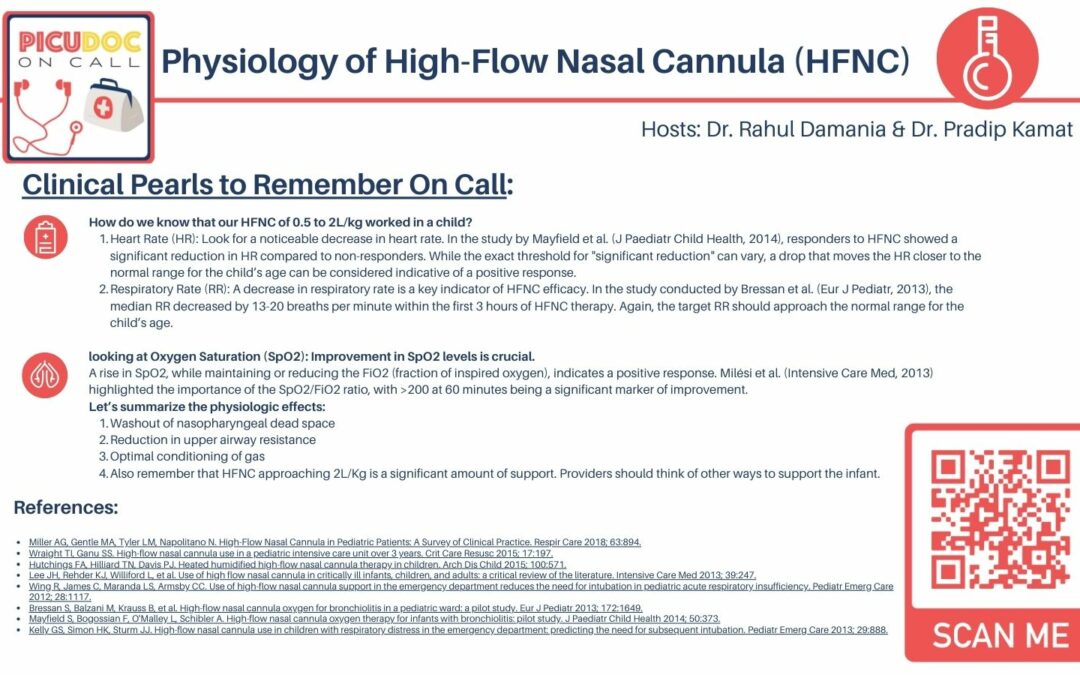
Washout of Nasopharyngeal Dead Space:
- HFNC clears nasopharyngeal dead space, improving oxygen efficiency.
- Reduces re-breathing of CO2 from the anatomical dead space.
- Enhances ventilation efficiency and oxygenation.
Reduction in Upper Airway Resistance:
- HFNC reduces resistance in the upper airway.
- Delivers rapid gas flow matching or exceeding natural inhalation rate.
- Eases breathing, especially in neonates and infants with narrow airways.
Optimal Conditioning of Gas:
- HFNC delivers heated and humidified oxygen, matching the body’s conditions.
- Reduces energy expenditure and risk of airway irritation
- More comfortable and effective compared to cold, dry air delivery
Debunking the PEEP Theory (Positive End-Expiratory Pressure)
- HFNC generates minimal and variable PEEP.
- Amount of PEEP depends on factors like flow rate and cannula size
- Not as high or consistent as other respiratory support devices
Research Findings
- A 2022 CHEST study by Khemani et al. on children with bronchiolitis challenged the conventional understanding of HFNC’s mechanisms.
- HFNC primarily reduces breathing effort but does not consistently increase lung volume (EELV) or tidal volume (VT).
- Reduction in the pressure rate product (PRP) indicates decreased breathing effort, but not significant alterations in EELV or VT.
Physiological Effects
- HR, RR, and SpO2 are key indicators of HFNC efficacy.
- HR and RR should approach normal ranges for the child’s age.
- Improvement in SpO2 levels while maintaining or reducing FiO2 indicates a positive response.
Conclusion
- HFNC is a valuable tool in pediatric care for alleviating respiratory distress.
- Not a one-size-fits-all solution; vigilant monitoring and reassessment are crucial
- Recognizing HFNC’s mechanisms allows for optimized bedside application.
Closing Remarks:
- Subscribe, share feedback, and leave a review on the podcast.
- Visit picudoconcall.org for more episodes and management cards.
- Hosted by Dr. Pradip Kamat and Dr. Rahul Damania
References
Wraight TI, Ganu SS. High-flow nasal cannula use in a pediatric intensive care unit over 3 years. Crit Care Resusc 2015; 17:197.
Hutchings FA, Hilliard TN, Davis PJ. Heated humidified high-flow nasal cannula therapy in children. Arch Dis Child 2015; 100:571.
Lee JH, Rehder KJ, Williford L, et al. Use of high flow nasal cannula in critically ill infants, children, and adults: a critical review of the literature. Intensive Care Med 2013; 39:247.
Wing R, James C, Maranda LS, Armsby CC. Use of high-flow nasal cannula support in the emergency department reduces the need for intubation in pediatric acute respiratory insufficiency. Pediatr Emerg Care 2012; 28:1117.
Mayfield S, Bogossian F, O’Malley L, Schibler A. High-flow nasal cannula oxygen therapy for infants with bronchiolitis: pilot study. J Paediatr Child Health 2014; 50:373.