Welcome to PICU Doc on Call, a podcast dedicated to current and aspiring intensivists. I’m Pradeep Kumar coming to you from Children’s Healthcare of Atlanta, Emory University School of Medicine, and I’m Rahul Damania from Cleveland Clinic Children’s Hospital. We are two pediatric ICU physicians passionate about all things medical education in the PICU.
Episode Overview:
PICU.com call focuses on interesting PICU cases and management in the acute care Pediatric setting. In this episode, we discuss the case of an eight-year-old boy with chest pain, fatigue, and shortness of breath. This case presentation by Rahul highlights the complexity of pediatric care in the PICU.
Case Presentation:
An eight-year-old boy with up-to-date immunizations and no recent travel or pet exposure presented to the PICU with chief complaints of chest pain, fatigue, and decreased oral intake. His history over the preceding two weeks included a diminishing appetite, episodes of vomiting, and shortness of breath.
On examination, he exhibited various cardiac findings, including a hyperdynamic left ventricle, murmurs, and a noted gallop. Abdominal and neurological findings were also concerning. Diagnostic studies revealed an enlarged heart, and sinus tachycardia with left ventricular hypertrophy, and echocardiography confirmed severe valvular and ventricular abnormalities.
Laboratory Findings:
Laboratory findings included elevated BNP, slightly elevated troponin, and elevated inflammatory markers (ESR and CRP). Strep throat culture was negative, but ASO and anti-DNAse B titers were markedly elevated. MRI confirmed multiple punctate infarctions, likely due to valvular heart disease.
Diagnosis:
Given the complex multisystem presentation, the child was admitted to the PICU for intensive monitoring and comprehensive management of this multisystem pathology. The working diagnosis is rheumatic fever.
The episode is organized into three parts:
- Pathophysiology of Acute Rheumatic Fever
- Approach to Diagnosis and Investigations
- Management and Prevention
Pathophysiology of Acute Rheumatic Fever:
Acute rheumatic fever is an autoimmune disease initiated by a response to group A strep infection, primarily due to molecular mimicry. The streptococcal M protein has structural similarities with host proteins, leading to organ damage, especially in the heart.
Epidemiology:
Acute rheumatic fever is most prevalent in low to middle-income areas, affecting over 80% of cases. It mainly affects children between 5 to 14 years of age, and overcrowded households and limited healthcare access increase the risk. Globally, rheumatic heart disease affects millions of people annually and claims many lives.
Jones Criteria for Diagnosis:
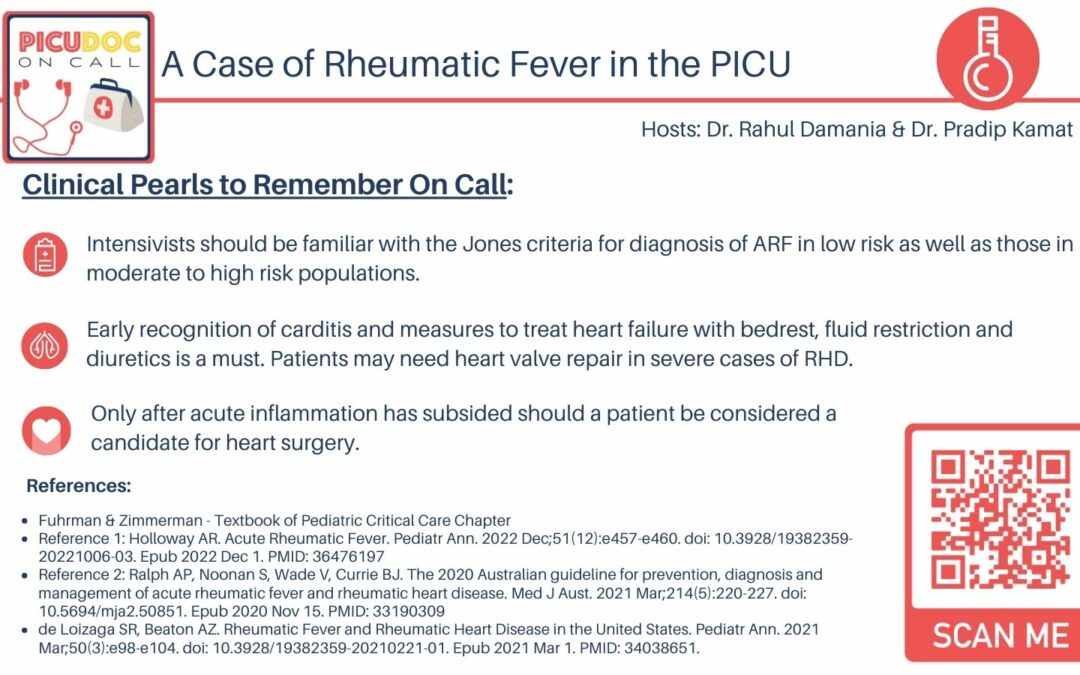
The Jones criteria help diagnose acute rheumatic fever. For a definitive diagnosis, evidence of a preceding group A strep infection is required. Major manifestations include carditis, arthritis, erythema marginatum, subcutaneous nodules, and Sydenham’s chorea. Minor criteria include fever, elevated inflammatory markers, prolonged PR interval on EKG, and mild joint issues.
Differentiating Low and High-Risk Populations:
The criteria differentiate between low and high-risk populations based on the epidemiology of acute rheumatic fever. The presentation of arthritis varies, and the thresholds for fever or inflammatory marker elevation are lower in high-risk populations.
Diagnostic Approach:
Diagnosis includes throat swab, anti-streptolysin O antibody titers, anti-DNAse B titers, CBC with differential, blood cultures, inflammatory markers, EKG, chest X-ray, and echocardiography. Joint analysis may be performed if needed.
Sydenham’s Chorea:
Sydenham’s chorea is marked by involuntary movements, primarily in the trunk and limbs, and it often resolves within 12 to 15 weeks with treatment.
Management of Acute Rheumatic Fever:
Management includes eradicating the remaining strep infection, controlling inflammation, and preventing recurrence. Penicillin or amoxicillin is used to treat the infection, while aspirin or NSAIDs are used to manage inflammation. In severe cases, systemic steroids may be considered. Cardiac surgery should be delayed until acute inflammation resolves. Prophylactic antibiotics are used for prevention.
Conclusion:
Rheumatic fever management requires a holistic approach, encompassing infection control, inflammation management, and long-term prevention. Early recognition, thorough diagnostics, and prophylactic antibiotics play essential roles in managing this condition.
Future Directions:
Research is needed for early detection using biomarkers and the development of a group A strep vaccine.
Closing Remarks:
As pediatric intensivists, we play a pivotal role in primary prevention by advocating for awareness and prompt treatment of group A strep infections.
Thank you for listening to PICU Doc on Call. Please subscribe, share your feedback, and visit our website at picudoconcall.org for more information. Stay tuned for our next episode.