Introduction:
Welcome to “PQ Doc On Call,” a podcast dedicated to current and aspiring intensivists. Hosted by Dr. Pradeep Kamar from Children’s Healthcare of Atlanta, Emory University School of Medicine, and Dr. Rahul Damia from Cleveland Clinic Children’s Hospital, both passionate PICU physicians.
You will hear:
This episode dives into the management of pediatric drowning cases in the PICU, providing valuable insights into assessment, pathophysiology, and practical management strategies.
Case Presentation:
An 18-month-old girl was admitted to the PICU following a submersion incident in a residential pool. The child’s initial unresponsiveness and subsequent clinical deterioration presented challenges for the PICU team, including respiratory distress, electrolyte imbalances, and potential neurological complications.
Key Elements from the Case:
- Severe acute respiratory failure following submersion
- Abnormal electrolytes (hyponatremia)
- Neurological insult requiring ongoing monitoring
Definitions and Terminology:
Clarification of drowning terminology, emphasizing uniform definitions and avoiding outdated terms like “near drowning.” Key terms include primary vs. secondary drowning, saltwater vs. freshwater, intentional vs. non-intentional, and fatal vs. non-fatal drowning incidents.
Pathophysiology:
- Airway Reflexes: Initial reflex laryngospasm triggered by liquid penetration, followed by relaxation due to hypoxia, hypercarbia, and acidosis.
- Gas Exchange Compromise: Decreased functional residual capacity leading to impaired oxygen uptake and CO2 elimination.
- Pulmonary Complications: Pulmonary edema, surfactant washout, increased pulmonary vascular resistance, and shunting, impacting oxygen delivery.
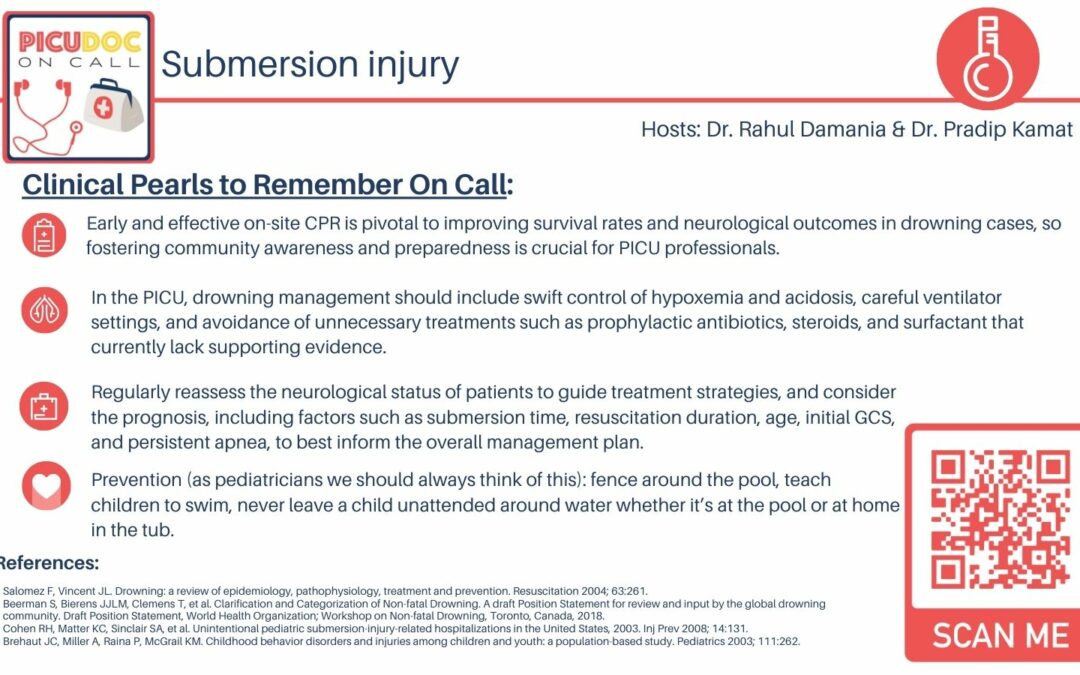
Management Strategies:
- Out-of-Hospital: Aggressive on-site CPR and advanced life support are crucial for favorable outcomes. Swift control of hypoxia and acidosis is vital.
- In-PICU: Ventilation strategies resembling ARDS management (low tidal volume, low plateau pressures, high PEEP). Consider neurological exam, continuous EEG, and neuromuscular blockade if needed.
- Prognostic Factors: Duration of submersion, time to effective CPR, initial GCS, apnea persistence, pH levels, and neurologic status.
Prevention:
Empowering prevention through measures like fencing around pools, teaching children to swim, and vigilant adult supervision can significantly reduce the risk of pediatric drowning incidents.
Conclusion:
“PQ Doc On Call” underscores the importance of timely, effective CPR, swift management of hypoxia and acidosis, and vigilant neurological assessment in pediatric drowning cases. Prevention remains paramount in avoiding such incidents.
Stay tuned for more engaging episodes from PICU Doc On Call! Don’t forget to subscribe, share your feedback, and review the podcast on your preferred platform. For more information and resources, visit picudoconcall.org.