Welcome to PICU Doc On Call, a podcast dedicated to current and aspiring intensivists. My name is Pradip Kamat.
My name is Rahul Damania, a current 2nd-year pediatric critical care fellow. We come to you from Children’s Healthcare of Atlanta-Emory University School of Medicine.
Today’s episode is dedicated to pediatric post-cardiac arrest care.
We are going to split this topic into two episodes, part one of pediatric post-cardiac arrest syndrome will address the epidemiology, causes, and pathophysiology.
I will turn it over to Rahul to start with our patient case…
- 11 yo previously healthy M who is admitted to the PICU after cardiac arrest.
- The patient was noted to be found unresponsive and submerged in a neighborhood pool.
- He was pulled out by bystanders and CPR was started for 5 minutes with two rounds of epinephrine prior to achieving ROSC.
- During transport to the OSH, the patient developed hypotension requiring a continuous epinephrine infusion.
- His initial blood gas was notable for a mixed respiratory and metabolic acidosis:
- 7.0/60/-20
- His initial serum lactate was 6.8 mmol/L.
- He presents to the PICU with a temperature of 36.6, HR 130s, MAPs 50s on Epinephrine infusion at 0.03mcg/kg/min
- He is mechanically ventilated with notable settings PEEP of 10, FiO2 65%.
- The patient is taken to head CT which shows diffuse cerebral edema and diffusely diminished grey-white differentiation most pronounced in the basal ganglia.
Great Rahul, can you please comment on his physical exam & PMH?
- Important physical exam findings include an unresponsive intubated patient with a cervical collar and bilateral non-reactive pupils at 4mm. The patient received mechanical ventilation with coarse breath sounds. A heart exam revealed tachycardia with no murmur or gallop. The patient does not respond to stimuli, intermittent jerking movements of arms and legs were observed. There was no evidence of rash or trauma. No past medical history of seizures or any heart disease. No home medications or toxic ingestions are suspected.
So now he is transferred to the ICU, what did we do?
- An arterial line, central venous line, urinary catheter, esophageal temperature probe was placed. The patient was ventilated using a TV of 6cc/kg and a PEEP of 10 (FIO2 ~65%) to keep SPO2 >94%. The patient initially had runs of ventricular tachycardia for which lidocaine was used. Although the initial EKG showed mild QTc prolongation, it subsequently normalized and was considered to be due to his cardiac arrest and resuscitation. An echocardiogram revealed normal biventricular systolic function (on epinephrine) and also showed normal origins of the coronary arteries. Comprehensive Arrhythmia Panel did not identify a specific genetic cause for the patient’s sudden cardiac arrest. The patient was placed on continuous EEG, which demonstrated severe diffuse encephalopathy with myoclonic status likely from anoxic brain injury Patient was also started on Levetiracetam and valproic acid. Initial portable CT scan done on day # of admission showed diffuse cerebral edema and diffusely diminished gray-white differentiation (most pronounced in the basal ganglia). MRI was deferred due to patient instability.
The case we talked about highlights a patient who had a trigger that then resulted in cardiac arrest is common is one of the common reasons for admission to the PICU at Children’s hospitals whether from submersion injury, trauma, ingestion, cardiac arrhythmia, sepsis, etc. Can we start by defining post-cardiac arrest syndrome?
- Successful resuscitation from cardiac arrest results in a post-cardiac arrest syndrome, which can evolve in the days to weeks after the return of spontaneous circulation. The components of post-cardiac arrest syndrome are brain injury, myocardial dysfunction, systemic ischemia/reperfusion response, and persistent precipitating pathophysiology. Prior to 2008, the AHA pediatric advanced life support (PALS) guidelines focused chiefly on the prevention of cardiac arrest, immediate recognition of cardiac arrest, and provision of early CPR because outcomes of pediatric cardiac arrest were poor. The past decade has led to focused efforts by resuscitation experts to address specific pediatric post-cardiac arrest knowledge gaps. In the 2019 Aug issue of Circulation (Vol 140, issue 6) published a scientific statement from the American Heart Association, which summarizes the epidemiology, pathophysiology, management, and prognostication after the return of sustained circulation after cardiac arrest, and it provides consensus on the current evidence supporting elements of pediatric post-cardiac arrest care.
- In order to provide post-cardiac arrest care (PCAC), caregivers need to understand the phases of cardiac arrest. Can you give us more information on the phases of cardiac arrest care?
- Let me start by defining ROSC or return of spontaneous circulation: ROSC refers to a return of sustained circulation, which can include circulation that results either from a perfusing spontaneous heart rhythm or from the establishment of extracorporeal circulation with extracorporeal membrane oxygenation (ECMO).
- The immediate phase: the first 0 to 20 minutes after ROSC
- The early phase: the period after ROSC from 20 minutes up to 6 to 12 hours
- The intermediate phase: 12 to 72 hours
- The recovery phase: approximately 72 hours to day 7. Starts at different times for different patients; the timing may be influenced by factors such as cardiovascular function or use of targeted temperature management (TTM)
- The rehabilitation phase: traditionally began with the application of care after discharge from the acute care hospital, but rehabilitation services are now often initiated during the intermediate phase or the recovery phase.
- What is the epidemiology of post-cardiac arrest syndrome (PCAS)?
- The timing and severity of the phases of post-cardiac arrest syndrome (PCAS) may differ between patients with out-of-hospital cardiac arrest (OHCA) and those with in-hospital cardiac arrest (IHCA) because witnessed status, preexisting conditions, cause of arrest, and timing and quality of bystander actions, such as immediate administration of high-quality CPR, may differ between OHCA and IHCA.
- It is estimated that >5000 children experience OHCA annually in the United States with an estimated incidence of non-traumatic OHCA of 8.04 per 100 000 person-years.11 With current ROSC rates of ≈36%. The reported survival to discharge in OHCA remains poor- 6.7-10.2% although favorable neurological outcome has been reported in 77% of pediatric OHCA survivors. One study using PECARN data (Moler FW et al. CCM 2011) of TTM in comatose children who survived OHCA to be admitted to a pediatric intensive care unit (ICU), reported that 38% survived to hospital discharge.
An estimated 6000 infants and children develop IHCA annually. Non–risk-adjusted ICU ROSC occurred in 78%, with 45% surviving to discharge; 89% of survivors had a favorable neurological outcome (Berg RA et al. CCM 2016)
Approximately 6500 children per year in the US have PCAS. The goal of PCAC is to increase not only survival to hospital discharge but also survival with favorable neurological outcomes.
- Can we take a deeper dive into the pathophysiology of PCAS? Let’s start with brain injury
- Post–cardiac arrest brain injury remains a leading cause of morbidity and mortality in adults and children because the brain has limited tolerance of ischemia, hyperemia, or edema. The first 3 phases of PCAS involve hypoxemic-hypotensive perfusion with energy deprivation. With ROSC, there is a burst of reactive oxygen species, and oxidative stress may ensue in tissue that is depleted of antioxidants. As a result, reperfusion is associated with excitotoxicity, calcium accumulation, and free radical-mediated cell injury or death. The myoclonic status seen in your case is probably due to this excitotoxicity. Both neuronal cellular necrosis and apoptosis result from this cascading injury and can continue in the days to weeks after ROSC.
- A variety of post-cardiac arrest clinical conditions, including hyperoxia, hypoxemia, and hypotension, can exacerbate the neuronal injury.
- What about cardiac injury in PCAS?
- Global myocardial dysfunction occurs even in the absence of a cardiac cause of the arrest, and the severity of the myocardial dysfunction may be related to the duration of no-flow time during cardiac arrest. Myocardial dysfunction has been associated with early mortality despite successful initial resuscitation in children and adults. The onset of post-cardiac arrest myocardial dysfunction begins within hours of the arrest, peaks at ≈8 hours, begins to improve at 24 hours, and typically resolves within 48 to 72 hours. The pathophysiology contributing to this frequently reversible deterioration of cardiac function after cardiac arrest is not fully understood but is associated with cardiovascular ischemia/reperfusion injury, cytokine-mediated cardiovascular dysfunction, and induced myocardial injury secondary to catecholamines or electric shocks. (Adrie C et al. Circulation 2002).Children may initially demonstrate a hyperdynamic state and then develop cardiac dysfunction over time. Because myocardial dysfunction is likely to develop in approximately two-thirds of patients after ROSC and subsequently improve, it is thought to be a modifiable risk factor.
Clinical manifestations of myocardial dysfunction include hypotension, left ventricular and RV systolic or diastolic dysfunction resulting in reduced cardiac output, arrhythmias, and pulmonary edema, which can result in recurrent cardiac arrest. Cardiac arrhythmias such as Vtach noted in the patient in your case are common during PCAC and may be exacerbated by catecholamine administration, which is required to maintain adequate cardiac output.
- Rahul**: What about systemic ischemia/reperfusion ?**
- The combination of systemic ischemia/reperfusion produces a state similar to the sepsis syndrome, with elevated cytokines, the presence of endotoxin in plasma, activation of coagulation pathways, and inhibition of anticoagulant pathways. Transient critical illness hyperglycemia occurs after cardiac arrest from a relative insulin-resistant state that is associated with high levels of endogenous catecholamines and cortisol secretion, with resulting gluconeogenesis and glycogenolysis. In children, the serum glucose is typically elevated in the first 12 to 18 hours after the insult and then falls to normal. Clinical manifestations of systemic ischemia/reperfusion include capillary leak with intravascular hypovolemia, vasoplegia, coagulopathy, hyperglycemia, adrenal insufficiency, and impaired oxygen utilization and delivery, contributing to multisystem organ dysfunction. I would like to advise our listeners that management of the child after cardiac arrest includes diagnosis and treatment of the precipitating cause of cardiac arrest. Failure to identify and correct the original cause of cardiac arrest leaves the patient at risk for secondary injury and even recurrence of cardiac arrest. A team approach using experts from cardiology, genetics, infectious disease, radiologists and toxicologists, etc., may be required to investigate the cause of cardiac arrest.
To summarize, the combination of systemic ischemia/reperfusion produces a state similar to the sepsis syndrome, with elevated cytokines, the presence of endotoxin in plasma, activation of coagulation pathways, and inhibition of anticoagulant pathways. Transient critical illness hyperglycemia occurs after cardiac arrest from a relative insulin-resistant state that is associated with high levels of endogenous catecholamines and cortisol secretion, with resulting gluconeogenesis and glycogenolysis. In children, the serum glucose is typically elevated in the first 12 to 18 hours after the insult and then falls to normal.
- Let’s discuss monitoring typically used in patients with PCAS?
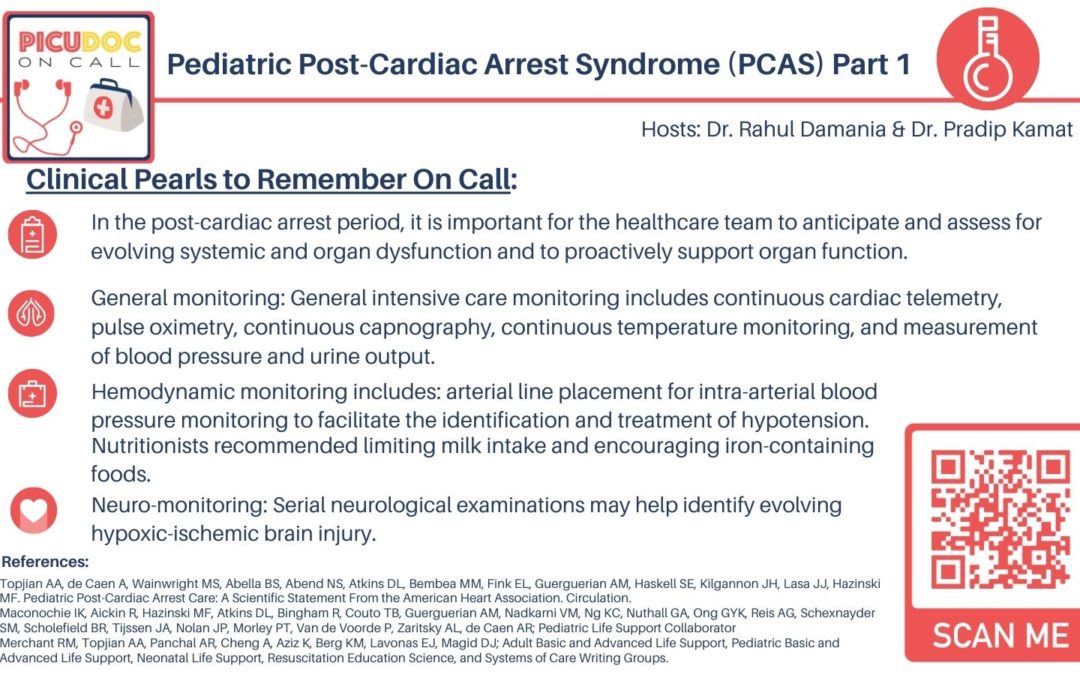
- In the post-cardiac arrest period, it is important for the healthcare team to anticipate and assess for evolving systemic and organ dysfunction and to proactively support organ function. This requires ongoing monitoring to guide intensive care therapies. Monitoring in the field continues through transport and includes ECG, pulse oximetry, capnography, noninvasive blood pressure measurement, and point-of-care glucose testing.
- General monitoring: General intensive care monitoring includes continuous cardiac telemetry, pulse oximetry, continuous capnography, continuous temperature monitoring, and measurement of blood pressure and urine output. Monitoring includes laboratory analysis of venous or arterial blood gases, serum electrolytes, and glucose and calcium concentration. Arterial lactate and central venous oxygen saturation assist in evaluation of the adequacy of tissue oxygen delivery. A chest x-ray aids evaluation of endotracheal tube position, heart size, and pulmonary status.52 Additional monitoring includes evaluation of renal function, measurement of hemoglobin concentration, monitoring of coagulation function, and assessment for signs of inflammation and infection.
- Hemodynamic monitoring includes: arterial line placement for intra-arterial blood pressure monitoring to facilitate the identification and treatment of hypotension. In addition, central venous catheters may be useful to monitor central venous oxygen saturation and to provide a route for the administration of fluids and medications. Pulmonary artery catheters are now rarely used in pediatrics. An echo and ECG should be performed. The optimal timing or frequency of echo acquisition remains unknown.
- Neuro-monitoring: Serial neurological examinations may help identify evolving hypoxic-ischemic brain injury. Given the high incidence of electrographic seizures after ROSC(Abend NS et al. Neurology 2011) monitoring with an electroencephalogram (EEG) is increasing in pediatric PCAC. Neuroimaging can be helpful to identify a cerebral cause of cardiac arrest and the presence of severe brain injury. One small pediatric study (36 patients) by Lee JK et al (Resuscitation 2014) evaluated the role of cerebral autoregulation in guiding hemodynamic management and oxygen delivery and assisting in neuroprognostication in comatose children after cardiac arrest, but more studies are needed.
This concludes our episode today on PCAS. We hope you found value in this short podcast. We welcome you to share your feedback & place a review on our podcast. PICU Doc on Call is co-hosted by Dr. Pradip Kamat, and my cohost Dr. Rahul Damania.
Stay tuned for our next episode which covers Part 2 of PCAS focused on Management! Thank you