Welcome to PICU Doc On Call, A Podcast Dedicated to Current and Aspiring Intensivists.
I’m Pradip Kamat and I’m Rahul Damania. We are coming to you from Children’s Healthcare of Atlanta – Emory University School of Medicine.
Welcome to our discussion today on airway clearance in the critically-ill patient in the PICU. We will focus on the use of pharmacological as well as non-pharmacological techniques in critically ill children admitted to the ICU. This episode will be a general overview as specific clinical scenarios such as NM disease may warrant specific therapeutics.
Let’s get started with the case:
We have an 8-month old ex-34 week premie intubated for acute respiratory failure secondary to RSV bronchiolitis. The patient is on a conventional mechanical ventilator receiving a TV of 6ml/kg, rate of 20, PEEP 6, 40% FiO2 inspiratory time of 0.7
CXR shows a pattern suggestive of viral pneumonia with minimal hyperinflation and atelectasis of the right middle lobe. The patient has excessive secretions when the suction catheter is assessed. The patient is hemodynamically stable and is on feeds via a NG tube.
Rahul, Can you comment on how a child clears his/her pulmonary secretions normally when not ill?
That’s an excellent question. Normally some baseline secretions are produced by all humans. Normal bronchial secretions are made up of contributions from mucus-secreting (goblet)cells as well as cells secreting serous fluid. The ciliary epithelium made of columnar cells line the entire tracheobronchial tree up to the alveolar ducts. This ciliary epithelium provides the coordinated rhythmic force that propels the overlying “mucus blanket” towards the central airways and upper respiratory tract.
Primary mechanisms of tracheobronchial clearance of these secretions consist of (1) The mucociliary (MC) escalator in the smaller airways and (2) Cough in central and larger airways. The co-ordinating activity of the beating cilia and their interaction with the overlying viscoelastic layer of mucus makes up the mucociliary escalator. The MC escalator helps remove both healthy and pathologic secretions from the airways as well as the removal of inhaled particles. This MC transport can be affected by mycoplasma, influenza and other viruses as well as exposure to toxins (cigarette smoke, vaping) as well as in CF, asthma, COPD, and ciliary dyskinesia just to name a few.
Once the secretions are in large or central airways they are coughed out or swallowed.
Let’s transition and talk a little on how one generates an effective cough:
- For an effective cough one needs firstly to take a sufficiently deep breath in.
- The glottis needs to close briefly to allow an increase in intrathoracic pressure
- This is followed by expulsive glottic opening together with abdominal contraction, which results in air being forcibly expelled.
Individuals with neuromuscular disease, bulbar insufficiency, obtunded patients, those on MV with chemical neuromuscular blockade, severe skeletal deformity may have decreased cough expiratory airflow. Reduced ability to cough results in secretion retention, mucus plugging, atelectasis and pre-disposition to infection even if the MC escalator function is normal.
Q2. Pradip can you tell us about atelectasis
This is a great question. The term atelectasis means “imperfect expansion” and indicates reversible loss of aerated lung with otherwise normal lung parenchyma.
Thats a nice concise definition, so if atelectasis reperesents imperfect expansion, what are mechanisms which keep our lungs open?
There are three major mechanisms:
1. Pulmonary Surfactant
2. Collateral Ventilation
3. Lung & Chest Wall Balance
Let’s go into each of these in more detail:
A pulmonary surfactant that covers the large alveolar surface is composed of phospholipids (mostly phosphatidylcholine), neutral lipids, and surfactant-specific apoproteins (termed surfactant proteins A , B , C , and D ). By reducing alveolar surface tension, pulmonary surfactant stabilizes the alveoli and prevents alveolar collapse.
There is a collateral ventilating mechanism (intra-alveolar pores & bronchiole-alveolar communications) that prevents alveolar collapse. Inter-alveolar pores by which alveoli are connected to each other via are called the Pores of Kohn. There also exist connections between distal bronchioles and neighboring alveoli called channels of Lambert. These structures can aerate hundreds of alveoli adjacent to a bronchiole preventing the collapse of one in case there is resorption of the air from that alveolus. Resorption occurs when an airway becomes occluded, the air is trapped in lung units ventilated by that airway, and the trapped gases are absorbed by the blood perfusing that part of the lung. Oxygen is absorbed faster than nitrogen from the alveolus into the blood resulting in collapsed lungs postoperatively especially if high O2 concentrations are used.
The balance between Inward recoil of lung tissue and outward expansion of the chest wall (myo-elastic element: smooth muscle fibers interwoven with elastic fibers in distal airways and alveolar sacs) is is opposed by an outward recoil of the chest wall. An exact balance of these forces is essentially FRC at end of exhalAnion. An imbalance of these forces which keep lungs open can predispose to atelectasis. An example of chest wall inability to provide outward recoil is the reason a patient with pneumothorax develops lung collapse
Awesome, let’s quickly summarize, atelectasis represents airway collapse, in order to keep alveoli open, our body’s mechanisms include pulmonary surfactant, collateral ventilation, and FRC.
Let’s transition and talk about the various types of atelectasis and the diseases we encounter in the PICU which can create an imperfect expansion of the alveoli?
Surfactant deficiency or dysfunction: Infant with surfactant deficiency or neonate with prematurity.
- Children with ARDS or Near drowning, as well as hydrocarbon ingestion, can all have surfactant dysfunction which can lead to atelectasis.
Resorption atelectasis (most common): high FIO2 concentration, intra-bronchial obstruction due to inflammation, infection, mucus plugs, and foreign body.
Another mechanism is an extrinsic compression of the small airways. c) Compression of normal lung tissue: Pleural effusion, chylothorax, cardiac enlargement or tumors, Extra bronchial compression: vascular ring, lobar emphysema or by lymph nodes
All in all, when you have atelectasis you run the risk of having decreased lung compliance, impairment of oxygenation, increased pulmonary vascular resistance, and development of lung injury.
In asthma and bronchiolitis, the right middle lobe and the lingula segment are the most common localization of the atelectasis and this is called the middle lobe syndrome. It is possible that hilar Lymph node enlargement due to viral infection and subsequent compression of middle lobe bronchus may be a cause of its preferred location.
Pradip, what are the clinical consequences of atelectasis?
This is a great question, and like many processes, clinical consequences Depend on the patient’s age, rate of formation, extent and of course the underlying cause of the atelectasis, however, let’s talk in general:
Going back to our case, a critically -ill patient such as an intubated infant with bronchiolitis on moderate ventilator settings, development of atelectasis can lead to rapid deterioration. This is contrasted, In a clinically stable child admittedly postoperatively for a non-pulmonary reason who is on RA, a significant atelectasis may go completely unnoticed and detected only on a chest radiograph.
5) Rahul how is atelectasis treated in the PICU patient admitted for acute illness (i.e without chronic neuromuscular condition)?
One of the primary approaches to tackle atelectasis involves Airway clearance or chest physiotherapy or pulmonary toilet (an outdated term) refers to a spectrum of physical and mechanical interventions aimed at interacting therapeutically with acute and chronic respiratory disorders.
Over the next few minutes we will cover some primary approaches, ranging from suctioning to manual CPT. To start,
One of the simplest modality is suctioning. In infants and toddlers with small ETT tubes transport of secretions may be hampered by the size of the ETT. Sedation/NMB use may diminish the cough reflex. So the suction acts like a cough substitute. Type of catheter, its size, depth of insertion are all standardized and moist centers gave their own policies/procedures. Pre-oxygenation prior to suctioning or mechanical hyperinflation post suctioning can also be used.
Another useful technique is postural drainage which is easily achieved in intubated patients: Gravity helps mobilize and transport secretions. If the atelectasis is in the right lung, then placing the patient in a left lateral decubitus position so that the right side is up will help open the right lung. This can be helped with chest percussion (RTs cupped hands or small cushioned mask or mechanical percussion devices), vibration, and even compression. I use this technique in small infants, and toddlers especially if they are intubated.
That’s great and I should add that it is important to have a sedation management plan or algorithm adequately balanced to the patient’s needs during these interventions.
Additionally, gentle bagging-(sometimes with saline lavage)-leading to an increase in lung volume and manual hyperinflation may help open a lung segment up. We need to be careful not to de-recruit the lung by frequent disconnection of the ventilator to do bag-lavage.
Pradip what are some of the mechanical devices you use in the PICU to help conventional chest physiotherapy?
This is a great question and to be honest, each type of chest PT has its risks and benefits, lets’s review the most common. We will talk about:
- IS
- IPV
- Mechanical In Ex (Cough Assist)
- Flutter/Acapella
- Vest therapy
Incentive spirometry (IS): The basis of incentive spirometry involves having the patient take a sustained, maximal inspiration (SMI). An SMI is a slow, deep inspiration from the FRC up to the total lung capacity (TLC) followed by ≥5 seconds breath hold. An incentive spirometer is a medical device that facilitates SMI. The device gives the individual visual feedback regarding flow and volume and also prevent and reverse atelectasis when used appropriately and regularly.
Patients who are at risk for developing atelectasis due to immobility especially post-operatively may be helped by the use of incentive spirometer. It can help improve lung volume, optimize oxygenation and maintain inspiratory muscle strength. One study by Fahd et al (Journal of Pediatric Hematology/Oncology) reported that mandatory IS for sickle cell disease patients admitted without respiratory complaints reduces transfusions and acute chest syndrome, particularly for those presenting with back pain.
IPV: Intrapulmonary percussive ventilator: The IPV device delivers high-flow jets of air to the airways by a pneumatic flow interrupter at a rate of 100 to 300 cycles/min through a mouthpiece. The patient controls variables such as inspiratory time, peak pressure, and delivery rates. IPV has been shown to be beneficial for secretion clearance (particularly for cystic fibrosis patients) and improvement in atelectasis in intubated patients.
Mechanical insufflator-exsufflator: CoughAssist is a portable, electric mechanical insufflation-exsufflation device that attempts to simulate a cough by using a blower and valve to alternately apply a positive and then a negative pressure to a patient’s airway to assist the patient in clearing retained bronchopulmonary secretions.
Flutter and Acapella devices are small, handheld devices that provide positive expiratory pressure (PEP). Exhaling through the device creates oscillations in the airway, resulting in loosening of mucus.
Percussive vests: A high-frequency chest wall vibrating/oscillating vest device has been shown to mobilize secretions in patients with cystic fibrosis and is commonly used as an adjunct airway clearance device in children with a reduced ability to clear secretions due to neuromuscular abnormalities
Rahul can you comment on some pharmacological approaches in the PICU?
Saline: 0.9% saline enables clearance of secretions, especially in an intubated patient. 0.9% saline loosens secretions, lubricates the ETT, enhances cough as well as decreases viscosity of the secretions. Studies are mixed as to the benefit of using saline instillation prior to suctioning in intubated patients.
One pediatric RCT (Riddling DA et. al. Am J Crit Care 2003) in postoperative patients with congenital heart disease showed no benefit with regard to incidence of VAP or mucus plugging. They also found (similar to adult studies) a drop in SpO2 from baseline in the group that used saline.
Hypertonic Saline: Although shown to be beneficial in children with cystic fibrosis who are > 6 years of age, One study showed no benefit in children under 6 years of age.
In bronchiolitis HS is believed to help by decreasing airway edema and thinning of mucus to alleviate plugging via the osmotic effect of HS. Literature about 3% HS has been conflicting at best with some studies showing benefit with regards to the length of stay and symptom score and others showing no benefit.
A 2017 Cochrane database review published by Zhang et al reported that nebulised hypertonic saline may modestly reduce length of stay among infants hospitalised with acute bronchiolitis and improve clinical severity score. Treatment with nebulised hypertonic saline may also reduce the risk of hospitalisation among outpatients and emergency department patients. However, we assessed the quality of the evidence as low to moderate. Quality of evidence is moderate due to substantial clinical heterogeneity between studies and large multicenter trials are still warranted.
Yes, Pradip, actually — One PICU randomized study by Shein et al (2016) reported on 18 intubated patients (9 in each group)- receiving either hypertonic saline or 0.9%NS used 4 times a day for 7 days. They found no difference in any outcomes measures between the two group after adjustment for baseline differences in respiratory parameters.
So Pradip, I have heard of N-Acetylcysteine or Mucomyst used as a pharmacological — how does it work?
N-acetylcysteine (mucomyst) : It hydrolyzes the disulfide bonds of mucins and other proteins. The sodium salts of NAC may also disrupt DNA. Animal studies suggest there may be some benefit to the airway due to its antioxidant effect, its use in ARDS has not shown any benefit although in one study in pediatric burn patients, the combination NAC and heparin resulted in lower rates of reintubation, atelectasis, and mortality. (Desai MH et al. J burn care rehabilitation).
What about Dornase Alpha?
Dornase alfa: is a recombinant human DNAase, which degrades DNA of the neutrophils, which migrate to the airway in inflammatory conditions. DNA from neutrophils increases the viscosity of the sputum and mucus plugging in the airway. Dornase decreases mucus viscosity and helps its clearance from the airway.
A Cochrane database review from 2018 (Yang et al)reported improved lung function in patients with cystic fibrosis in trials lasting from one month to two years. There was a decrease in pulmonary exacerbations in trials of six months or longer. A meta-analysis from 2012 (Enriquez et al.) reported no benefit with respect to clinical scores in patients with bronchiolitis but longer duration of hospitalization.
Nebulized heparin has been used in burn patients. It changes the rheology of sputum, elasticity of the mucus, and may have antibacterial effects on certain pathogens. It has been shown to enhance the effect of Dornase in CF patients.
As a summary, many of these pharamacological agents are best studied in the CF population, and I think the literature is mixed in other populations especially the PICU.
Rahul, what about the role of bronchoscopy in secretion clearance?
Bronchoscopy can be used for secretion clearance from the airways especially in patients with a head injury who are at risk for intracranial hypertension from non-pharmacologic airway clearance techniques such as IPV or percussive vest therapy. Bronchoscopy also allows for the ability to get a biological specimen for gm stain/Cx. Bronchoscopy can also help reveal cause of atelectasis such as extrinsic compression of airways due to cardiomyopathy or from tenacious mucous plugging etc. Additionally, bronchoscopy can help with instillation of mucolytics into the airways.
As we close, let’s take an extreme example, say we have a patient intubated for ARDS that escalates to HFOV. What are the clinical pearls for airway clearance in this circumstance?
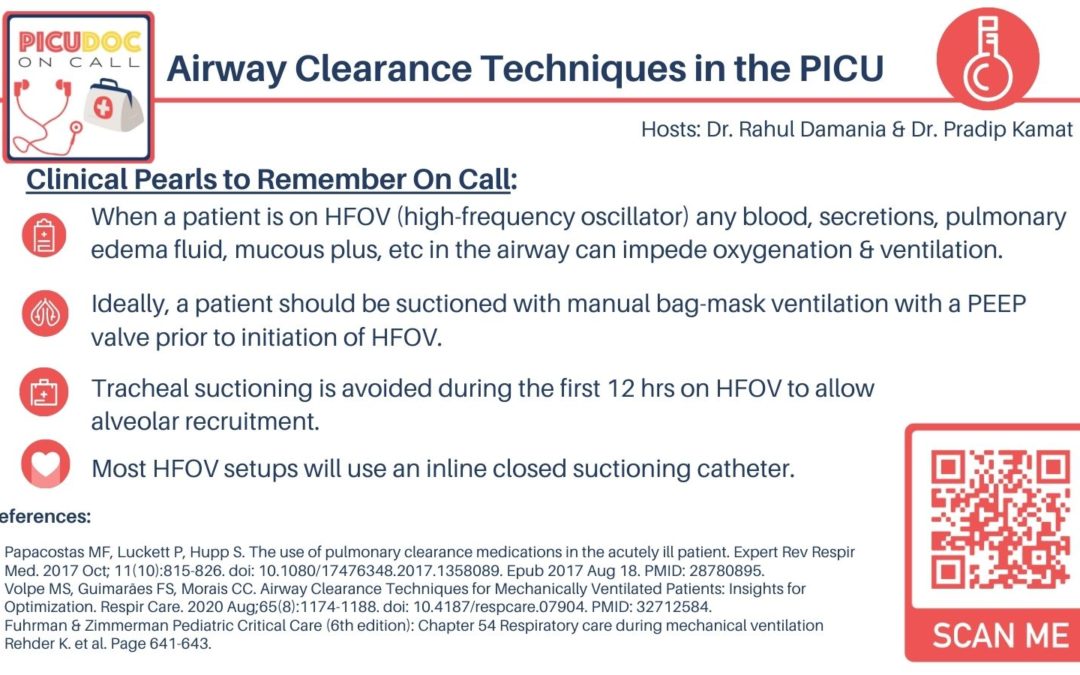
First of all, when a patient is on HFOV (high-frequency oscillator) any blood, secretions, pulmonary edema fluid, mucous plus, etc in the airway can impede oxygenation & ventilation.
Ideally, a patient should be suctioned with manual bag-mask ventilation with a PEEP valve prior to initiation of HFOV. Sometimes bronchoscopy may be indicated prior to recruitment using HFOV.
Tracheal suctioning is avoided during the first 12 hrs on HFOV to allow alveolar recruitment.
Most HFOV setups will use an inline closed suctioning catheter just like in a conventional ventilator but “routine scheduled” suctioning is avoided unless there is suspicion of ETT occlusion etc in order to prevent de-recruitment.
During HFOV sometimes suctioning maybe required for acute occlusion of ETT due to secretions, which will manifest as decreased wiggle, rising PCO2, hypoxia and increasing FiO2 requirement. Open suctioning using saline with bag-mask ventilation should be attempted only briefly after taking patient off HFOV in above conditions. Lung recruitment using a higher mean airway pressure may be required following the suctioning to prevent de-recruitment.
Rahul, can you comment on additional practical strategies used in the PICU ?
I think limiting sedation, NMB, would be helpful. Additionally, Lots of PICU’s are now following the SCCCM’s ICU liberation bundle, which includes early mobility, and assessing extubation readiness would help get the patient off the ventilator faster.
As a summary there is a limited role for routine pharmacological & non-pharmacological airway clearance in acute-ill PICU patients. Exceptions can be made on a case by case bases. However assistance with airway clearance is critical for reducing morbidity and mortality in children with neuromuscular weakness and those with cystic fibrosis.
References:
Papacostas MF, Luckett P, Hupp S. The use of pulmonary clearance medications in the acutely ill patient. Expert Rev Respir Med. 2017 Oct; 11(10):815-826. doi: 10.1080/17476348.2017.1358089. Epub 2017 Aug 18. PMID: 28780895.
Volpe MS, Guimarães FS, Morais CC. Airway Clearance Techniques for Mechanically Ventilated Patients: Insights for Optimization. Respir Care. 2020 Aug;65(8):1174-1188. doi: 10.4187/respcare.07904. PMID: 32712584.
Fuhrman & Zimmerman Pediatric Critical Care (6th edition): Chapter 54 Respiratory care during mechanical ventilation Rehder K. et al. Page 641-643.
This concludes our episode on airway clearance techniques We hope you found value in our short, case-based podcast. We welcome you to share your feedback, subscribe & place a review on our podcast! Please visit our website picudoconcall.org which showcases our episodes as well as our Doc on Call management cards. PICU Doc on Call is co-hosted by myself Dr. Pradip Kamat and Dr. Rahul Damania. Stay tuned for our next episode! Thank you!