Welcome to PICU Doc On Call, A Podcast Dedicated to Current and Aspiring Intensivists.
I’m Pradip Kamat and I’m Rahul Damania and we are coming to you from Children’s Healthcare of Atlanta – Emory University School of Medicine.
Welcome to our Episode of a 16 year old with fever and a rash.
Here’s the case:
A 16 year old F presents to the PICU with generalized weakness, fever and a diffuse rash**.** Three days prior to admission she stated that she was feeling lightheaded and the day after she started having frequent non-bloody diarrhea. She states that she has otherwise been healthy, no sick contacts or travel, and the only change in her life was her menstrual cycle which ended a few days before her symptoms started. She says that about two weeks ago, she went to her primary care physician to get an in-grown toe nail drained, but was able to recover after some analgesia and antibiotics for a week. On day of admission her mother brings her into the ED as she says her rash continues to progress. Her mother states that the rash looks like a sunburn. Mother noticed on day of admission that her daughter now had red injected eyes bilaterally without discharge, and was becoming increasingly confused with her fevers. Of note, the patient has also has had decreased oral intake as she says her mouth quote hurts when she swallows. She has had no sore throat, congestion, dysuria, or headache. She presents to the ED febrile to 39 C and tachycardic to 130 bpm. She is ill appearing and has orthostatic vital signs. Her exam is notable for palpable diffuse myalgia, oropharyngeal hyperemia, diffuse erythroderma, and conjunctival injection. She is noted to have a hyperdynamic precordium and faint crackles bilaterally. Her L toe is mildly erythematous with no discharge, necrosis or pain to palpation. Acute resuscitation and diagnostics are begun and patient is transferred to the pediatric intensive care unit.
To summarize key elements from this case, this patient has:
- Hx of a fever and multisystem involvement including GI manifestations, myalgias, confusion, mucositis, and rash
- This is in the setting of a local drainage procedure and course of antibiotics.
- In addition, she presents now with fever, hypotension, and tachycardia.
- These elements so far bring up a broad differential but for now we can agree that it seems that she has signs of acute inflammation or infection throughout her body.
nsition into some history and physical exam components of this case.
- If we take a step back, what are key history features in a child who presents with fever & rash?
- Understanding the characteristics of the rash, the evolution, and progression of the rash is important.
- In the setting of myalgias, fever, headache, and rash you should think of assessing for any recent travel as tick-borne illnesses commonly present with this symptomatology.
- You also want to assess for recent antibiotic exposures, sexual history, and surgical history – in our case, our patient had a recent procedure on her toe
- Are there some red-flag symptoms or physical exam components which you could highlight?
- Absolutely, when a child presents with fever and a rash, it is important to stratify two major elements:
- You want to assess the degree of toxicity in relation to the symptomatology:
- Lethargy, irritatbility, altered sensorium, poor perfusion, pallor or cyanosis may indicate serious illness.
- Understanding the duration of fever in the setting of suspected total body inflammation is important, however the importance of the heigh of fever in predicting the risk of serious illness is unclear.
- We will visit a differential a bit later in this podcast, however I do want to highlight that the presence of tachycardia and tachypnea in any patient with fever and rash suggests the possibility of sepsis.
- When you notice these red-flag symptoms it is important to focus on resuscitation and treatment rather than pursuing diagnostics.
- To continue with our case, our patients labs were consistent with:
- An AKI – with her creatinine being three times the upper limit of normal.
- A transaminitis and indirect hyperbilirubinemia.
- Thrombocytopenia
- Pyuria on UA with negative LE or nitrites.
- And finally, an elevated CPK at 2000 units/L.
- Looking ahead in this case, our patient had negative serologies for RMSF, leptospirosis, measles.
Ok, to summarize, we have:
- 16 yo F who presents with fever, diffuse erythroderma, signs of systemic inflammation, and multi-organ dysfunction all of which bring up concern for Toxic Shock Syndrome, the topic of our discussion today.
- Let’s start with a short multiple choice question:
- A patient presents with fever and rash and concern for Staphylococcal Toxic Shock Syndrome. Which of the following describes the mechanism of pathogenesis behind this diagnosis?
- A. Increased TLR-4 binding with LPS.
- B. Endotoxin production.
- C. Increased MHC II binding with T-cell receptor.
- D. Cytokine release of TGF-beta and IL-10.
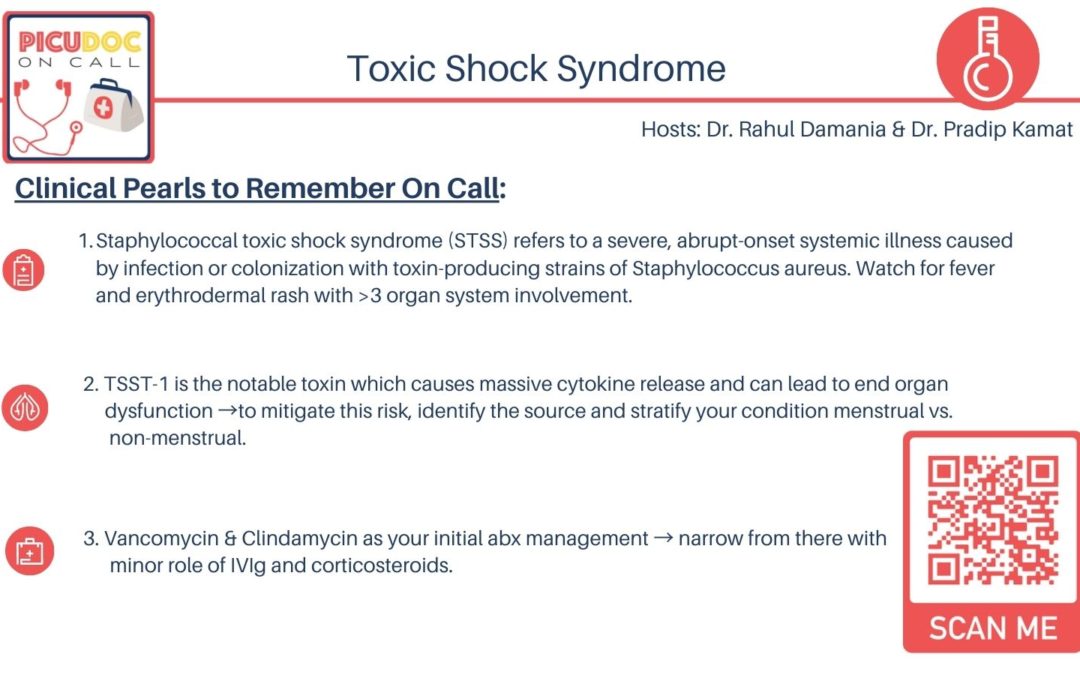
- The answer is C. Increased MHC II binding with T-cell receptor. Staphylococcal Toxic Shock Syndrome characteristically has a TSST-1 exotoxin which is present in all of menstrual cases toxic shock syndrome and about half the non-menstrual cases of toxic shock syndrome. The interaction and stabilization between the antigen presenting cells and T-cell receptors cause a massive cytokine storm and thus this superAg can be one of the major virulence factors behind the multi-system involvement we see in toxic-shock-syndrome. Interestingly, one of the cytokines which is released in this syndrome is TNF and this inhibits neutrophil function. Data suggests that TSST-1 in addition to TNF do not engender Staph to have a purulent response and this may be due to lack of PMN recruitment.
- As you think about our case, what would be your differential?
- This is an interesting differential however given her symptomatology and disease progression I would focus my differential to infectious entities first. These include but are not limited to:
- Disseminated Meningococcemia ( type of rash, lack of meningismus)
- Rocky Mountain Spotted Fever (type of rash, exposure/travel history)
- Leptospirosis (type of rash/ exposure to rodents feces and urine)
- Dengue fever (bleeding besides arthralgias and rash)
- Typhoid fever
- Now Staph Scalded skin syndrome may have similar nomenclature and pathogenesis as TSS however they are slightly different. A review article published in Clinical Infectious Diseases in 2006, highlighted key differences between SSS and TSS. These included:
- Age — as patients with TSS are older with a median age of 12 years compared to 4 years with SSS.
- Presence of bullae that rupture with light pressure (i.e. are nikolsky sign +) due to SSS’s exofoliative toxin.
- And lack of mucous membrane involvement which can stratify this from TSS and other severe exfoliative skin conditions.
- Sepsis or septic shock due to other pathogens is important to have at the top of your differential. Gram negative, fungal pathogens, or culture negative sepsis may clasicilly not be associated with rash but making the empiric diagnosis at the bedside upon presentation is key.
- Ok so we covered differentials related to fever and rash that are infectious in nature. Are there other broad categories to consider?
- Yes, inflammatory causes are important to also pursue:
- Drug reactions may have fever, systemic symptoms, and dermatological involvement. These include Steven Johnsons syndrome (SJS), Toxic epidermal necrolysis (TEN), or DRESS syndrome.
- I would also add COVID-19 related multi inflammatory syndrome to our differential and its close mimicker Kawasaki disease.
- Especially when a child presents with a prodrome of fever for 5 days and systemic signs of inflammation, you should think about Kawasaki disease and also its severe manifestations, namely myocarditis.
- That was a great differential. Before we continue, we want to revisit some key points from our case that narrowed our differential to Staphylococcal Toxic shock syndrome and cover some brief points regarding this condition:
- Firstly, we classically are tested in board exams of the retained tampon leading to TSS however in actuality menstrual cases of TSS are on the decline. This decrease may be explained by the withdrawal of highlight absorbent tampons and the absence of polyacrylate rayon-containing products from the market. Nonetheless, doing a pelvic exam is important to assess for retained tampons.
- At least half of reported Staphylococcal TSS cases are not related to menstruation and thus a variety of clinical circumstances can be associated. In our case, post procedure or surgical wound infections can be a trigger but the literature also cites burns and even respiratory infections such as the flu. In a report of 5300 TSS cases over a decade, the proportion of TSS cases following surgical procedures increased from 15 percent to about 27 percent. The case-fatality rate for non menstrual TSS was 5%.
- Secondly I want to highlight Streptococcal TSS. Surgical triggers may be common in history but in diving into the literature it seems that Streptococcal TSS has more of a virulent nature. These patients present with:
- Myonecrosis and a necrotizing fasciitis picture often with no visible break in the skin.
- They can have coagulopathy liver dysfunction and ARDS
- Typically you will isolate GAS from a normally sterile site but I wanted to highlight this phenomena as these patients can present with vascular collapse!
Let’s conclude by going through a diagnostic and management framework for TSS:
- If you had to work up this patient with TSS, what would be your diagnostic approach?
- Routine blood tests:
- CBC’d
- CMP
- Lactate
- Blood gas
- & coagulation studies is where I would start
- In our case with myositis getting a CK is reasonable
- Microbiological testing including 2 sets of blood cultures, UA, urine cultures, and as mentioned blood cultures will be important.
- I would also consider getting a wound culture if there is a surgical site abnormality along with inflammatory markers.
- Key point It is important to do a pelvic exam and nasopharyngeal exam to isolate any foreign or retained bodies as you want to really establish source control
- Of note, blood and sterile site cultures are positive for S. aureus in <5% of toxic shock cases, and testing for TSST is typically an academic exercise.
- If our history, physical, and diagnostic investigation led us to Toxic Shock Syndrome as our diagnosis what would be your general management of framework?
- Great question, I first off want to say that there have been none to very few randomized trials or evidence-based guidelines defining treatment regimens.
- You will not go wrong in the early stages to parallel the management of septic shock. This includes:
- Aggressive fluid resuscitation use of vasopressors or inotropes
- Initiation of broad spectrum antibiotics
- Supportive measures such as mechanical ventilation or renal replacement therapy when indicated. In a paper published in Annals of IM in 2005, renal dysfunction and central nervous system involvement are common and may occur more often in non menstrual TSS
- I think a key element here is to support end organ dysfunction and also treat the underlying cause – in this case it is the source control.
- What antibiotic regimen would you recommend:
- Clindamycin with Vancomycin can be an initial therapy.
- Studies have cited that the addition of clindamycin as a protein synthesis inhibitor can have the potential to suppress toxin production. Clindamycin is often added for its in vitro ability to suppress toxin production as well as evidence that clindamycin may reduce mortality in patients with streptococcal toxic shock syndrome. This was well defined in an older study published in 1997 which showed toxic shock syndrome toxin-1 (TSST-1) production is completely inhibited by clindamycin in logarithmic and stationary phase growth.
- Excellent review on this, I would also encourage clinicians to consult Pediatric Infectious Disease as their invaluable expertise & following of culture data is crucial.
- Once you get culture data, you can narrow to more MSSA tailored antibiotics like:
- Nafcillin or oxacillin
- Is there a role for IVIg?
- No trials evaluating use in staphylococcal toxic shock syndrome have been identified. However there have been case reports showing efficacy in streptococcal toxic shock syndrome. In vitro data shows that Staph aureus superantigens are less effectively inhibited by IVIG than streptococcal Ag. The Red Book suggests that there could be a potential role for IV Ig in patient with fluid refractory TSS as IVIg may play a role in neutralizing toxin. You should consider this in patients who are critically ill, unresponsive to fluid resuscitation, an undrainable infection, pulmonary edema, and oliguria.
- And finally to add, Use of corticosteroids therapy is controversial. There seems to be a potential survival benefit in animal models.
- Invitro studies show that dexamethasone suppresses TSST-1-induced cytokine production. In a study published in 1984 in JAMA, early adjunctive treatment with corticosteroids may be associated with reduced severity and duration of toxic shock syndrome symptoms but not decreased mortality. The current AAP Red Book does not mention a role for steroids.