Welcome to PICU Doc On Call, a podcast dedicated to current and aspiring intensivists. My name is Pradip Kamat
and my name is Rahul Damania and we come to you from Children’s Healthcare of Atlanta Emory University School of Medicine. Today’s episode is dedicated to the rational use of antibiotics in the PICU
We are delighted to be joined by two brilliant Pediatric clinical pharmacists Ms Whitney Moore and Ms. Stephanie Yasechko from Children’s Healthcare of Atlanta.
I will turn it over to Rahul to start with our patient case…
- Case
An 8-year-old female (24 kg, 130 cm) with PMH significant for severe persistent asthma and history of multiple PICU admissions presents to the ED with swelling, redness and inability to bear weight in her (L) lower leg.
Patient had just finished soccer practice the evening prior to her ED visit when she first noticed swelling and redness of her left lower leg. She also had a fever as well as some non-bloody, non-bilious emesis. Her past h/o is significant for poorly controlled asthma with multiple admissions to the PICU.
Upon arrival to the ED, patient’s BP was hypotensive, tachycardic, and tachypneic. She was given two 20 mL/kg NS boluses, and blood cultures were drawn in addition to a CBC, BMP, and UA.
Labs were notable for an elevated white count, lactate, and serum Cr. Patient was given a dose of antibiotic, and transported to the PICU for further workup and management.
Whitney and Stephanie welcome to PICU Doc on call.
Thanks Rahul and Pradip for having us. Neither one of us have any financial disclosures or conflicts of interest.
We want to divide today’s discussion into 3 segments- antibiotic selection, transition into dosing and end with therapeutic monitoring
Whitney, what are some of the factors to consider prior to choosing an antibiotic regimen in our patient case with a preliminary diagnosis of cellulitis of the left lower extremity with possible sepsis?
- Whitney: First and foremost you want to consider your host so really diving deep into the patient’s past medical history and secondly we should consider the likely pathogens that are causing the patient’s infection. In this case given the invasive nature of her infection and recent hospital admissions I would start Vancomycin and Cefepime. Once blood cultures results are back, we can then tailor or narrow her antibiotics based on susceptibilities.
Stephanie what are some of the other factors to consider prior to starting antibiotics in this patient?
- Other things to consider include her multiple previous hospitalizations, significant exposure to broad-spectrum antibiotics, whether or not she is immunocompromised, the presence of chronic conditions like lung disease, ventilator/trach dependency, and if patient was a resident of a long term care facility. Additionally any history of organ or bone marrow transplant or malignancy with use of chemotherapy/radiation, and/or a history of growth of multiple drug resistant organisms.
This is an important point – infectious disease is not just about the relevant pathogen or “bug” but it is also about understanding the host status!
Stephanie -why vancomycin and cefepime in this case?
- In this patient the major pathogens to consider include: P. aeruginosa (give her multiple previous PICU admissions).
- Also she has extensive cellulitis which necessitates antibiotic coverage against Methicillin resistant staph aureus (MRSA) and Streptococcus pyogenes . So our options in this case include vancomycin for broad-spectrum gram positive coverage, and generally either piperacillin/tazobactam or cefepime for broad-spectrum gram negative and pseudomonal coverage.
- As you can see by patient’s Scr, it appears that she is presenting in AKI since we have no history of her having any type of renal impairment at baseline; therefore, to minimize additional AKI risk, cefepime would be our most appropriate choice for the time being. There is literature that shows us that the combination of vancomycin and piperacillin/tazobactam specifically has a much higher risk of AKI than other nephrotoxic combinations and should be avoided if possible.
Whitney lets now transition from abx selection to dosing — how would you dose vancomycin and cefepime in our patient case?
- An appropriate dose of vancomycin to start out here would be 15 mg/kg, with a maximum of 1000 mg. However, instead of scheduling a defined frequency, pharmacy would recommend a x1 dose, and check a level in a couple of hours in patients who present with any type of unstable renal function. However, traditional vancomycin dosing in patients with normal renal function is either 20 mg/kg/dose IV every 8 hours or 15 mg/kg/dose IV every 6 hours with a max of 1000 mg/dose.
- Cefepime is traditionally dosed at 50 mg/kg/dose IV every 8 hours; however, since our patient has AKI, we should calculate her CrCl or estimated GFR to renally adjust the dose. As you all know there are a couple of equations we could use to calculate her clearance. But the modified Bedside Schwartz equation is the gold standard for pediatric patients. Once the GFR or CrCl is calculated we can then adjust the dose for her AKI.
I think this is a great time to start to highlight the importance of collaboration between the intensivists, nursing & the pharmacy team. These children already are tenuous and as we treat with broad spectrum abx it is important to also consider the side effects such as nephrotoxicity of broad spectrum antibiotics.
As we discussed specifics of dosing of Vanc and Cefepime, Stephanie, if we take a step back what are some of the other factors to consider prior to antibiotic dosing?
- In terms of selecting the most appropriate dose, we always want to consider factors like age, weight, renal/hepatic function, as well as the area in the body we wish to penetrate (CNS, bone, blood, etc.).
- Additionally, it is very important to identify whether or not the patient is currently receiving continuous renal replacement therapy(CRRT), plasma exchange, ECMO, or fluids and/or diuretics, because all of these can affect drugs quite significantly from a pharmacokinetic standpoint.
- Lexicomp (available either as a paper-back or online) is the gold standard for pediatric dosing. And of course your clinical pharmacist specialist is always available to help with dosing references, and can provide recommendations on how to most appropriately dose your specific patient
Whitney how would you monitor the patient given evidence of AKI and the need for a nephrotoxic antibiotic such as vancomycin?
- Depending on the severity of the renal dysfunction, the vancomycin level can be checked anywhere from 8-24 hours post administration
- A therapeutic steady-state drug concentration is generally reached after the administration of about 3-4 doses (or 4 to 5 half-lives). The therapeutic goal trough level is 10-15 mcg/mL for all infections, except for those harder to penetrate areas like the CNS or the heart. In these cases the target trough is higher at 15-20 mcg/mL.
To summarize, those “hard to reach areas” such as the blood brain barrier or the heart — we should ensure a higher trough in order for us to reach therapeutic effect.
Stephanie, what are important points regarding trough monitoring for vancomycin?
- Trough monitoring represents a therapeutic controversy within the pharmacy community, as recent vancomycin dosing guidelines have changed to now recommend area under the curve (AUC) guided monitoring as the most efficacious and safe way to monitor the drug given its narrow therapeutic range and increased nephrotoxic risk with trough monitoring.
- Here at our institution, we have not yet fully incorporated this new monitoring technique. We are reserving AUC monitoring for patients with MRSA bacteremia or unable to achieve therapeutic troughs with traditional dosing.
This is a great practical example, as the bedside staff it is important to optimize communication as antibiotic troughs are time sensitive.
Now that we have discussed vancomycin, Stephanie what about dosing and monitoring of cefepime in our patient?
- Cefepime, does not require therapeutic drug monitoring, so determination of an appropriate dose is dependent on CrCL, and it is important to recognize that continuous adjustments may need to be made as renal function improves or declines.
- Refer to Lexicomp for all renal dose adjustments. Rule of thumb, if CrCL > 50, a patient can be dosed normally. Anything less should be evaluated.
Let’s wrap up this section by summarizing some important dosing points for Vancomycin and Cefepime. Whitney, as your patient improves how would you approach de-escalation of abx?
- There are two important points I want you to remember when dosing vancomycin and cefepime. First, is knowing the maximum dose of each medication. Cefepime we max the dose at 2000 mg per dose, and our initial starting dose maximum for vancomycin is 1000 mg, as mentioned. We can go up to 1250 but only after we have drawn levels and need to. But knowing the maximum dose is an important point to consider when dosing a large patient because you don’t want to exceed an adult dose. The second important point I want you to remember is calculating the patient’s clearance and adjusting the dose and/or frequency based on the patients renal function if needed.
- Now, in regards to de-escalation of antibiotics, once the patient is no longer septic, with a resolved AKI, and cultures and susceptibilities have resulted, the team will determine if a full treatment course is warranted or not. If it is, then broad-spectrum antibiotics can be discontinued, and we can narrow to an antibiotic that the patient’s pathogen is susceptible to.
This is an important point — narrowing broad spectrum antimicrobials optimizes antibiotic stewardship.
As we build on our case, Stephanie, if the blood culture grew Methicillin sensitive staph Aureus (MSSA) what antibiotic would be used and how will it be dosed?
- When a patient’s blood culture is positive for MSSA, it is considered an invasive infection. Most common sources of bacteremia include endocarditis, skin and soft tissue infections, intravascular catheter infections, bone and joint infections, pneumonia, etc. and in 25% there is no source.
- MSSA can give rise to sepsis syndrome and septic shock with a mortality of 10-20%.
- We typically use nafcillin or oxacillin 2 gm IV Q4 hours or even an infusion. One retrospective study reported that continuous oxacillin was an effective alternative to intermittent oxacillin for the treatment of infective endocarditis caused by MSSA and may improve microbiological cure.
- Cefazolin can also be used. Patients who cannot be treated with beta-lactams, should be administered vancomycin or daptomycin. For uncomplicated bacteremia, a two week regimen is used. For complicated infection we typically do a 4-6 week course.
- Finally, understanding that patients who have toxic shock syndrome from staphylococcal species, Clindamycin has been shown to have bacteriostatic effects and reduce production of bacterial toxins!
Key points: MSSA likes to form a biofilm especially on internal hardware, and continuous oxacillin may be an effective option for treatment prior to consider removing the hardware for source control.
Our final portion of this podcast relates to specific clinical scenarios. We will be covering broad spectrum therapy for specific patient populations. We will cover anti-microbial coverage for patients who have:
- Hematologic malignancies
- Solid organ transplant on immunosuppression
- Neontal sepsis
- Sickle cell
and …Children with:
- VP shunts
- Perforated appendicitis
- Lemierre’s disease
- …and finally the undifferentiated, critically ill, child.
Whitney lets start with patients who have an underlying hematologic malignancies. What would be an initial empiric anti-microbial regimen for these patients?
- We typically use Cefepime, or zosyn, for gram negative coverage to cover bugs like pseudomonas & enterobacteriaceae. And for enhanced Gram positive coverage for your staph and strep we add vancomycin especially if there is presence of a central line associated bloodstream infection (BSI), or if the patient has severe mucositis, a skin and soft tissue infection, pneumonia or is hemodynamically unstable).
- If the patients fever continues with no source identification by about day 5 (4 to 7 window), consider adding an antifungal agent like micafungin or caspofungin. And if patient happens to already be on an antifungal for prophylaxis, consider adding voriconazole.
And what about the the patient who has a solid organ transplant on immunosuppression who presents with septic shock?
- In transplant patients or those on immunosuppression we should first consider the fact that some immunosuppressive medications are known to be nephrotoxic and interact with other medications. Second thing we should consider like I mentioned before is our host. If they are immune compromised they will need broader coverage. Therefore, the most appropriate choices would be vancomycin and cefepime. If the patient continues to clinically decompensated, then it would be appropriate to add on that antifungal coverage with micafungin.
This is an important point – immuno-suppresants may compound end organ dysfunction and further, may have key drug interactions, such as CYP enzymes, which may alter your antimicrobial or antifungal kinetics.
Stephanie, let’s continue with our specific patient populations which antibiotics would we consider in neonatal sepsis?
- Ampicillin +Cefotaxime OR Ampicillin +gentamicin but given shortage of cefotaxime we should consider ampicillin with ceftazidime.
- We want to cover Group B streptococci, E Coli and other gram negatives along with listeria species.
- Discontinue antibiotics if cultures are negative after 48 hours and suspicion for infection is low based on inflammatory markers.
(Stephanie) What about the patient with fever, headache, altered sensorium concerning for bacterial meningitis, can you also comment on the patient with ventriculoperitoneal shunt infection and brain abscess?
- So in this scenario, it is essential to select antimicrobials that penetrate the CNS. Therefore, generally speaking, an appropriate selection would be vancomycin and ceftriaxone. The more inflamed the meninges are, the greater CNS penetration you are going to get with vancomycin. We would also add metronidazole for brain abscess to vancomycin and ceftriaxone to cover for anaerobic organisms.
The addition of Vancomycin combined with Ceftriaxone especially in patients who have meningitis and no hardware is important in overcoming resistant S. Pneumo strains.
Whitney, what is our coverage for perforated appendicitis with sepsis?
- For a perforated appendicitis with sepsis, piperacillin/tazobactam (Zosyn) is our preferred agent. Also the combination of Ampicillin +gentamicin + metronidazole can be used. When thinking of appendicitis you want to cover for your GI bugs like klebsiella, proteus, bacteroides and other anaerobes.
- One thing to note when thinking about gut coverage is clindamycin’s resistance to B. fragilis is increasing and is up to 60% worldwide, therefore, it’s no longer recommended for intra-abdominal infections.
Stephanie, What about neck abscesses and septic thrombophlebitis (such as Lemierre syndrome)
- A beta-lactamase resistant beta-lactam antibiotic (ampicillin/sulbactam) is recommended as an empiric therapy due to case reports of treatment failures with penicillin secondary to beta-lactamase producing F. necrophorum.
- Antibiotics should of course be tailored to the culture results and susceptibility data when available.
- Alternative options include clindamycin or metronidazole for patients with significant clinical allergy to beta-lactams. Clindamycin is preferred (for head, neck and lung anaerobic infections) as it has activity against metronidazole-resistant organisms such as actinomycetes and peptostreptococci.
(Allen BW, Anjum F, Bentley TP. Lemierre Syndrome. [Updated 2020 Dec 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499846.)
It is important for us to highlight that the likely microbe associated with Lemierre’s is Fusobacterium necrophorum!
Whitney, lets conclude with our final patient population. What is your typical coverage in patient with Sickle cell disease who presents with sepsis, or acute chest syndrome?
- Levofloxacin is our agent of choice in this scenario to provide routine bacterial coverage as well as atypical coverage. Traditionally we would have done a 3rd generation cephalosporin, but we try to avoid the empiric use of ceftriaxone due to the association with life threatening hemolysis after administration.
Though this incidence is rare, it is important to understand that CTX can cause intravascular hemolysis in these patients who already have compromised Oxygen delivery due to their anemia.
Alright Stephanie, we have reached the end of our episode today… but I have one more question, as a fellow, when I am on call and we have a previously healthy child who presents to the PICU who is critically ill and hemodynamically unstable, what antibiotics should we consider ?
- Once again, the concept of where exactly we think the source of the infection is will drive antibiotic selection with the goal of providing the best empiric therapy for the most likely pathogen(s). In a previously healthy patient who has really had no recent hospitalizations or antibiotic exposure, we could start with ceftriaxone. If the patient, however, has MRSA of PSE risk factors, at that point we would then need to broaden to vancomycin and either cefepime/ceftazidime/or piperacillin/tazobactam.
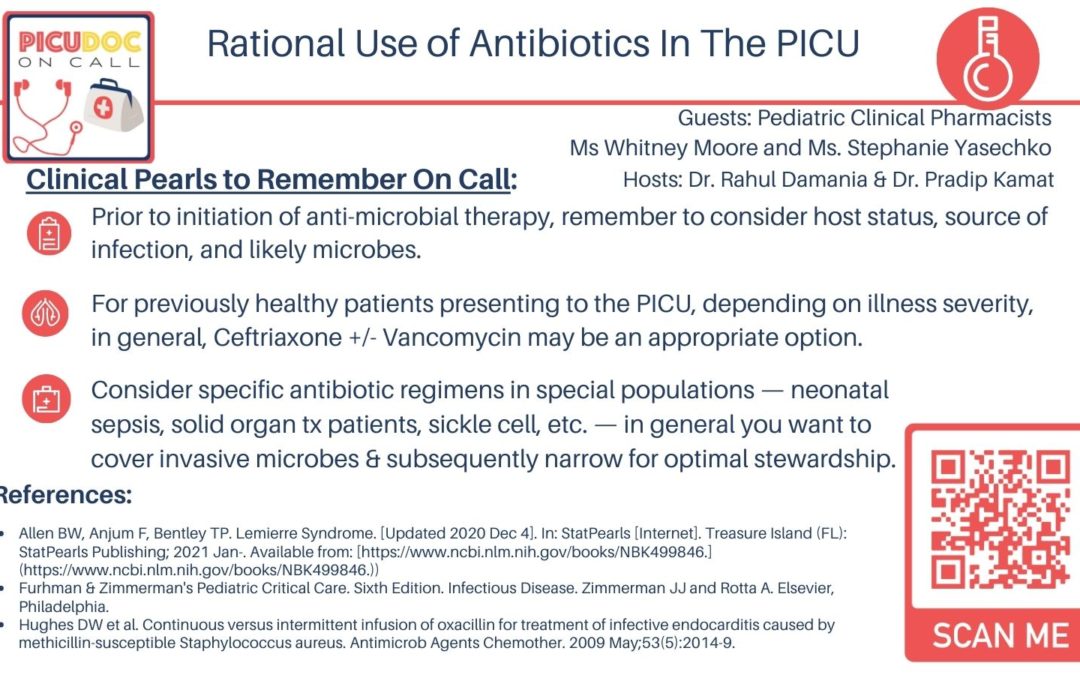
To take this episode home, remember to consider host status, source of infection, and likely microbes prior to initiation of broad spectrum therapy!
Whitney and Stephanie thank you so much for your expertise on common bugs and drugs — this was a great discussion, and we value your expertise. What are your take home clinical pearls for anti-microbials in the PICU..
Stephanie: Your clinical pharmacist can always help with choice of antibiotics as well as dosing and monitoring, especially in critically-ill children with AKI or hepatic dysfunction.
Whitney: The clinical pharmacists work very closely with the antimicrobial stewardship team and the infectious disease service to choose the optimal agent with least toxicity and potential to develop resistance.
Stephanie: Finally, have a multi-disciplinary approach to tailoring your antibiotics, consider host status, clinical course, and duration of broad spectrum therapy — and just as a plug, your pharmacists & infectious disease service members are more than happy to help you along this process!
This concludes our episode today on anti-microbials in the Pediatric Intensive Care Setting. We hope you found value in this short podcast as we delved into antimicrobial selection, dosing and special populations. We welcome you to share your feedback & place a review on our podcast! As always, PICU Doc on Call is co-hosted by myself, Dr. Pradip Kamat and Dr. Rahul Damania. Stay tuned for our next episode! Thank you.
Welcome to PICU Doc On Call, a podcast dedicated to current and aspiring intensivists. My name is Pradip Kamat
and my name is Rahul Damania and we come to you from Children’s Healthcare of Atlanta Emory University School of Medicine. Today’s episode is dedicated to the rational use of antibiotics in the PICU
We are delighted to be joined by two brilliant Pediatric clinical pharmacists Ms Whitney Moore and Ms. Stephanie Yasechko from Children’s Healthcare of Atlanta.
I will turn it over to Rahul to start with our patient case…
- Case
An 8-year-old female (24 kg, 130 cm) with PMH significant for severe persistent asthma and history of multiple PICU admissions presents to the ED with swelling, redness and inability to bear weight in her (L) lower leg.
Patient had just finished soccer practice the evening prior to her ED visit when she first noticed swelling and redness of her left lower leg. She also had a fever as well as some non-bloody, non-bilious emesis. Her past h/o is significant for poorly controlled asthma with multiple admissions to the PICU.
Upon arrival to the ED, patient’s BP was hypotensive, tachycardic, and tachypneic. She was given two 20 mL/kg NS boluses, and blood cultures were drawn in addition to a CBC, BMP, and UA.
Labs were notable for an elevated white count, lactate, and serum Cr. Patient was given a dose of antibiotic, and transported to the PICU for further workup and management.
Whitney and Stephanie welcome to PICU Doc on call.
Thanks Rahul and Pradip for having us. Neither one of us have any financial disclosures or conflicts of interest.
We want to divide today’s discussion into 3 segments- antibiotic selection, transition into dosing and end with therapeutic monitoring
Whitney, what are some of the factors to consider prior to choosing an antibiotic regimen in our patient case with a preliminary diagnosis of cellulitis of the left lower extremity with possible sepsis?
- Whitney: First and foremost you want to consider host (i.e. patient characteristics) and secondly we should consider the likely pathogens that are causing the infection. In this patient given the invasive nature if her infection I would start Vancomycin and cefepime. Once blood cultures results are back, we can then tailor (I.e narrow) the antibiotic used based on susceptibilities.
Stephanie what are some of the other factors to consider prior to starting antibiotics in this patient?
- Other things to consider include her multiple previous hospitalizations, significant exposure to broad-spectrum antibiotics, if she is immunocompromised or not, the presence of chronic conditions like lung disease or ventilator/trach dependence, and if patient was a resident of a long term care facility. Additionally any history of organ or bone marrow transplant or malignancy with use of chemotherapy/radiation, and/or a history of growth of multiple drug resistant organisms.
This is an important point – infectious disease is not just about the relevant pathogen or “bug” but it is also about understanding the host status!
Stephanie -why vancomycin and cefepime in this case?
- In this patient the major pathogens to consider include: P. aeruginosa (give her multiple previous PICU admissions).
- Also she has extensive cellulitis which necessitates antibiotic coverage against Methicillin resistant staph aureus (MRSA) and Streptococcus pyogenes . So our options in this case include vancomycin for broad-spectrum gram positive coverage, and generally either piperacillin/tazobactam or cefepime for broad-spectrum gram negative and pseudomonal coverage.
- However, as you can see by patient’s Scr, it appears that she is presenting in AKI since we have no history of her having any type of renal impairment at baseline; therefore, to minimize additional AKI risk, cefepime would be our most appropriate choice for the time being. There is literature that shows us the combination of vancomycin and piperacillin/tazobactam specifically has a much higher risk of AKI than other nephrotoxic combinations and should be avoided if possible.
Whitney lets now transition from abx selection to dosing — how would you dose vancomycin and cefepime in the our patient case?
- An appropriate dose of vancomycin to start out here would be 15 mg/kg, with a max of 1000 mg, but instead of scheduling a defined frequency, generally pharmacy recommends to do a x1 dose, and then check a level in patients who present with any type of unstable renal function to assess how well the patient is clearing the drug. However, traditional vancomycin dosing is 20 mg/kg/dose IV q8h or 15 mg/kg/dose q6h with a max of 1000 mg/dose with normal renal function.
- Cefepime is traditionally dosed at 50 mg/kg/dose every 8 hours; however, since our patient has AKI, we should calculate her CrCl or estimated GFR and renally adjust the dose. As you all know there are a couple of equations we could use to calculate her clearance; however, the modified Bedside Schwartz equation is the gold standard for pediatric patients. Once the eGFR is calculated you can adjust for her AKI.
I think this is a great time to start to highlight the importance of collaboration between the intensivists, nursing & the pharmacy team. These children already are tenuous and as we treat with broad spectrum abx it is important to also consider the side effects such as nephrotoxicity of broad spectrum antibiotics.
As we discussed specifics of dosing of Vanc and Cefepime, Stephanie, if we take a step back what are some of the other factors to consider prior to antibiotic dosing?
- In terms of selecting the most appropriate dose, we want to consider factors like age, weight, renal/hepatic function, as well as the area in the body we wish to penetrate (CNS, bone, blood, etc.).
- Additionally, it is very important to identify whether or not the patient is currently receiving Continuous renal replacement therapy(CRRT) or plasma exchange or ECMO, fluids, and/or diuretics because all of these can affect drugs quite significantly from a pharmacokinetic standpoint.
- Lexicomp (available either as a paper-back or online is the gold standard for pediatric dosing. And of course your clinical pharmacist specialist is always available to help with dosing references, and can provide recommendations on how to most appropriately dose your specific patient
Whitney how would you monitor the patient given evidence of AKI and the need for nephrotoxic antibiotic such as vancomycin?
- Depending on the severity of the renal dysfunction, the vancomycin level can be checked anywhere from 8-24 hours post administration.
- A therapeutic steady-state drug concentration is generally reached after the administration of 3-4 doses (or 4 to 5 half-lives), and goal trough levels are 10-15 mcg/mL for all infections, except for meningitis and endocarditis, where targets of up to 15-20 are generally preferred to ensure adequate CNS and cardiac penetration.
To summarize, those “hard to reach areas” such as the blood brain barrier or the heart — we should ensure a higher trough in order for us to reach therapeutic effect.
Stephanie, what are important points regarding trough monitoring for vancomycin?
- Trough monitoring represents a therapeutic controversy within the pharmacy community, as recent vancomycin dosing guidelines have changed to now recommend area under the curve (AUC) guided monitoring as the most efficacious and safe way to monitor the drug given its narrow therapeutic range and increased nephrotoxic risk with trough monitoring.
- Here at our institution, we have not yet fully incorporated this new monitoring technique. We are reserving AUC monitoring for patients with MRSA bacteremia or unable to achieve therapeutic troughs with traditional dosing.
This is a great practical example, as the bedside staff it is important to optimize communication as at times antibiotic troughs are time sensitive.
Now that we have discussed vancomycin, Stephanie what about dosing and monitoring of cefepime in our patient?
- Cefepime, does not require therapeutic drug monitoring, so determination of an appropriate dose is dependent on CrCL, and it is important to recognize that continuous adjustments may need to be made as renal function improves or declines.
- Refer to Lexicomp for all renal dose adjustments. Rule of thumb, if CrCL > 50, a patient can be dosed normally. Anything less should be evaluated.
Let’s wrap up this section by summarizing some important dosing points for Vancomycin and Cefepime. Whitney, As your patient improves how would you approach de-escalation of abx?
- Generally for cefepime we cap the dose at 2 grams per dose, and our initial starting dose maximum for vancomycin is 1 gram, as mentioned, which are also very important points to consider when dosing a large patient so that we are not going over adult maximum doses.
- Once this patient’s septic sho is no longer septic, with a resolved AKI, and cultures and susceptibilities have resulted, the team will determine if a full treatment course is warranted or not. If it is, then broad-spectrum antimicrobials can be discontinued, and the patient can continue on an agent that his/her pathogen is susceptible to.
This is an important point — narrowing broad spectrum antimicrobials optimizes antibiotic stewardship.
As we build on our case, Stephanie, if the blood culture grew Methicillin sensitive staph Aureus (MSSA) what antibiotic would be used and how will it be dosed?
- When a patient’s blood culture is positive for MSSA its is considered an invasive infection. Most common sources of bacteremia include endocarditis, skin and soft tissue infections, intravascular catheters infection, bone and joint, pneumonia etc and in 25% there is no source.
- MSSA can give rise to sepsis syndrome and septic shock with a mortality of 10-20%.
- We typically use nafcillin or oxacillin 2gm IV Q4 hours or even an infusion. One retrospective study reported that continuous oxacillin was an effective alternative to intermittent oxacillin for the treatment of infective endocarditis caused by MSSA and may improve microbiological cure.
- Cefazolin can also be used. Patients who cannot be treated with beta-lactams, should be administered vancomycin and daptomycin. For uncomplicated bacteremia a two week regimen is used. For complicated infection we typically do a 4-6 week course.
- Finally, understanding that patients who have toxic shock syndrome from staphylococcal species, Clindamycin has been shown to have bacteriostatic effects and reduce production of bacterial toxins!
Key points: MSSA likes to form a biofilm especially on internal hardware, and continuous oxacillin may be an effective option for treatment prior to consider removing the hardware for source control.
Our final portion of this podcast relates to specific clinical scenarios. We will be covering broad spectrum therapy for specific patient populations. We will cover anti-microbial coverage for patients who have:
- Hematologic malignancies
- Solid organ transplant on immunosuppression
- Neontal sepsis
- Sickle cell
and …Children with:
- VP shunts
- Perforated appendicitis
- Lemierre’s disease
- …and finally the undifferentiated, critically ill, child.
Whitney lets start with patients who have an underlying hematologic malignancies. What would be an initial empiric anti-microbial regimen for these patients?
- We typically use Cefepime (or meropenem) for Gram negative coverage ( enterobacteriaceae, pseudomonas) and for enhanced Gram positive coverage (staphylococci and streptococci) vancomycin is added (especially if there presence of central line associated bloodstream infection (BSI), severe mucositis, skin and soft tissue infection, pneumonia or hemodynamic instability).
- If fever continues with no source identification- day 4-7, consider adding an antifungal (micafungin or caspofungin), if patient was on antifungal prophylaxis, consider adding voriconazole.
And what about the the patient who has a solid organ transplant on immunosuppression who presents with septic shock?
- Immunosuppressive medications are known to be nephrotoxic and interact with other medications. Therefore, likely the most appropriate choices would be vancomycin and cefepime. If the patient continues to clinically decompensated, then it would be appropriate to add on antifungal coverage with micafungin.
This is an important point – immuno-suppresants may compound end organ dysfunction and further, may have key drug interactions, such as CYP enzymes, which may alter your antimicrobial or antifungal kinetics.
Stephanie, let’s continue with our specific patient populations which antibiotics would we consider in neonatal sepsis?
- Ampicillin +Cefotaxime OR Ampicillin +gentamicin but given shortage of cefotaxime we should consider ampicillin with ceftazidime.
- We want to cover Group B streptococci, E Coli and other gram negatives along with listeria species.
- Discontinue antibiotics if cultures are negative after 48 hours and suspicion for infection is low based on inflammatory markers.
(Stephanie) What about the patient with fever, headache, altered sensorium concerning for bacterial meningitis, can you also comment on the patient with ventriculoperitoneal shunt infection and brain abscess?
- So in this scenario, it is essential to select antimicrobials that penetrate the CNS. Therefore, generally speaking, an appropriate selection would be vancomycin and ceftriaxone. The more inflamed the meninges are, the greater CNS penetration you are going to get with vancomycin. We would add metronidazole for brain abscess to Vancomycin and ceftriaxone.
The addition of Vancomycin combined with Ceftriaxone especially in patients who have meningitis and no hardware is important in overcoming resistant S. Pneumo strains.
Whitney, what is our coverage for perforated appendicitis with sepsis?
- For a perforated appendicitis with sepsis, piperacillin/tazobactam is our preferred agent. Also Ampicillin +gentamicin + metronidazole can also be used.
- Clindamycin resistant to B. fragilis is increasing (60% worldwide) and is no longer recommended for intra-abdominal infections.
Stephanie, What about neck abscesses and septic thrombophlebitis (such as Lemierre syndrome)
- A beta-lactamase resistant beta-lactam antibiotic (ampicillin/sulbactam) is recommended as an empiric therapy due to case reports of treatment failures with penicillin secondary to beta-lactamase producing F. necrophorum.
- Antibiotics should of course be tailored to the culture results and susceptibility data when available.
- Alternative options include clindamycin or metronidazole for patients with significant clinical allergy to beta-lactams. Clindamycin is preferred (for head, neck and lung anaerobic infections) as it has activity against metronidazole-resistant organisms such as actinomycetes and peptostreptococci.
(Allen BW, Anjum F, Bentley TP. Lemierre Syndrome. [Updated 2020 Dec 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499846.)
It is important for us to highlight that the likely microbe associated with Lemierre’s is Fusobacterium necrophorum!
Whitney, lets conclude with our final patient population. What is your typical coverage in patient with Sickle cell disease who presents with sepsis, or acute chest syndrome?
- Levofloxacin is our agent of choice in this scenario to provide routine bacterial as well as atypical coverage. We would like to avoid the empiric use of ceftriaxone due to association with life threatening hemolysis.
Though this incidence is rare, it is important to understand that CTX can cause intravascular hemolysis in these patients who already have compromised Oxygen delivery due to their anemia.
Alright Stephanie, we have reached the end of our episode today… but I have one more question, as a fellow, when I am on call and we have a previously healthy child who presents to the PICU who is critically ill and hemodynamically what antibiotics should we consider ?
- Once again, the concept of where exactly we think the source of the infection is will drive antibiotic selection with the goal of providing the best empiric therapy for the most likely pathogen(s). In a previously healthy patient who has really had no recent hospitalizations or antibiotic exposure, we could start with ceftriaxone. If the patient, however, has MRSA of PSE risk factors, at that point we would then need to broaden to vancomycin and either cefepime/ceftazidime/or piperacillin/tazobactam.
To take this episode home, remember to consider host status, source of infection, and likely microbes prior to initiation of broad spectrum therapy!
Whitney and Stephanie thank you so much for your expertise on common bugs and drugs — this was a great discussion, and we value your expertise. What are your take home clinical pearls for anti-microbials in the PICU..
Stephanie: Your clinical pharmacist can help with choice of antibiotic, dosing and monitoring especially in critically-ill children with AKI or hepatic dysfunction
Whitney: The clinical pharmacists work very closely with antibiotic stewardship and infectious disease services to choose the optimal agent with least toxicity and potential to develop resistance.
Stephanie: Finally, have a multi-disciplinary approach to tailoring your anti-biotics, consider host status, clinical course, and duration of broad spectrum therapy — and just as a plug, your pharmacists & infectious disease are more than happy to help you along this process!
This concludes our episode today on anti-microbials in the Pediatric Intensive Care Setting. We hope you found value in this short podcast as we delved into antimicrobial selection, dosing and special populations. We welcome you to share your feedback & place a review on our podcast! As always, PICU Doc on Call is co-hosted by myself, Dr. Pradip Kamat and Dr. Rahul Damania. Stay tuned for our next episode! Thank you.
References:
- Allen BW, Anjum F, Bentley TP. Lemierre Syndrome. [Updated 2020 Dec 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: [https://www.ncbi.nlm.nih.gov/books/NBK499846.](https://www.ncbi.nlm.nih.gov/books/NBK499846.))
- Furhman & Zimmerman’s Pediatric Critical Care. Sixth Edition. Infectious Disease. Zimmerman JJ and Rotta A. Elsevier, Philadelphia.
- Hughes DW et al. Continuous versus intermittent infusion of oxacillin for treatment of infective endocarditis caused by methicillin-susceptible Staphylococcus aureus. Antimicrob Agents Chemother. 2009 May;53(5):2014-9.