Today’s episode is dedicated to the approach to thyroid storm. It’s the first in our Mini-Case series.
Show Highlights:
Our case, symptoms, and diagnosis: A 12-year-old female presents to the PICU with chest discomfort. She was noted to be anxious by her parents over the past few days. They felt she was a bit “off,” as she would constantly drop items and have a tremor. A few weeks prior to these symptoms, she was noted to have rhinorrhea, congestion, and progressive neck swelling. Her parents became increasingly concerned this morning as her temperature was 104F. Per her parents, she was agitated throughout the night and became increasingly somnolent in the early morning.
To summarize key elements from this case, this patient has:
- Chest pain likely due to a cardiac etiology or musculoskeletal cause.
- Tremor likely due to a primary neurologic cause or increased metabolic drive.
- Neck swelling with fever after a prodrome of URI symptoms which could be concerning for lymphadenitis or thyroid goiter.
- Synthesizing these symptoms together, this patient likely has a systemic etiology such as hyperthyroidism, with the most severe manifestation being thyroid storm, a toxidrome, or a pheochromocytoma. Given the fever and altered mental status, considering sepsis is key.
Key history features in this child with tachycardia and signs of hyperthyroidism:
- High fevers up to 104F
- Altered mental status
- Neck swelling
Red flag symptoms and physical exam components in a patient with severe hyperthyroidism include:
- Airway
- Check for dyspnea or stridor when the patient is supine.
- Do a Mallampati assessment.
- Auscultate for a bruit in the neck.
- Cardiovascular system
- Concerns include congestive heart failure and cardiac dysrhythmias.
- Widened pulse pressure is common
The American Thyroid Association has advocated for the Burch-Wartofsky Point Scale (BWPS) for severe thyrotoxicosis. A score of 45 or higher indicates thyroid storm. A case-control study published in 2015 in the Journal of Endocrinology noted that the BWPS may overdiagnose up to 20% of patients. Clinical criteria on the BWPS include the following:
- Thermoregulatory dysfunction
- Central nervous system effects
- Gastrointestinal-hepatic dysfunction
- Cardiovascular dysfunction
- Congestive heart failure
- Presence or absence of a precipitant history of URI or underlying thyroid condition
Back to our specific case, the patient’s labs are consistent with low TSH and elevated free T4, indicating primary hyperthyroidism, positive for TSH-receptor antibodies, and the diagnosis of thyroid storm was confirmed.
- Other lab findings included elevated WBC, high ALT and AST, elevated glucose, and elevated cortisol. Her cardiac evaluation was notable for sinus tachycardia with occasional PACs.
- Other important labs include a coagulation panel, BNP and lactate, CRP, procalcitonin, blood cultures, and basic blood chemistries.
Let’s quiz ourselves with a multiple choice question:
- A patient with thyroid storm is admitted to the PICU. He is started on thyroid modulating therapy. Which of the following mechanisms of action does this medication likely work by?
- A. Activate Thyroid Peroxidase
- B. Inhibit Thyroid Peroxidase
- C. Inhibit Iodine Uptake within the Thyroid
- D. Increase conversion from T4 to T3
The correct answer is B. The most likely medication which is used in thyroid storm is methimazole or propylthiouracil. Both of these medications block thyroid peroxidase.
In terms of differential in our case, you want to think about other causes of fever, tachycardia, and CNS dysfunction, including, but not limited to sepsis, serotonin syndrome, neuroleptic malignant syndrome, heatstroke, and drug intoxication.
The diagnostic approach for our patient should focus on her history and physical examination. Be sure to include thyroid function tests, cardiac evaluation via EKG or Echo, chest x-ray, blood culture, urine analysis, and lateral neck radiographs to assess airway compression.
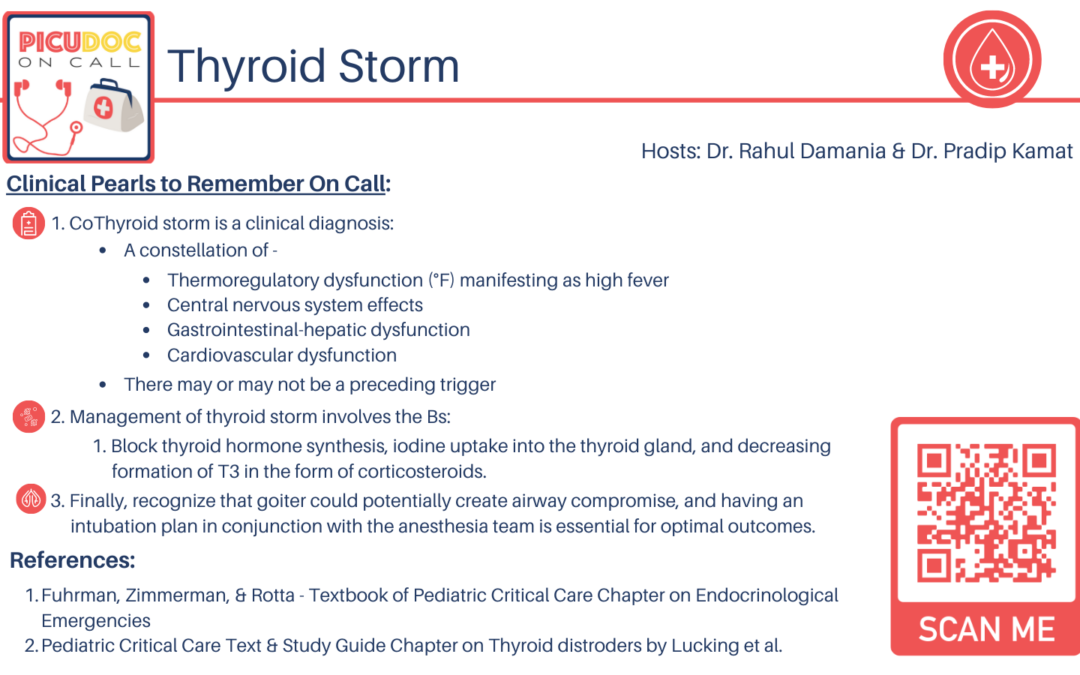
The general management framework for the diagnosis of thyroid storm should include a multimodal approach to block thyroid hormone production and action quickly, reverse systemic decompensation, and identify and treat any underlying causes and precipitants of thyroid storm. The key components are:
- Optimal communication between the pediatric endocrinology team and ICU staff
- Acute resuscitative measures in the PICU, such as aggressive cooling measures, IV fluids, and stress-dose steroids
- Management of thyroid storm is characterized by the “Five Bs”:
- Block synthesis of new thyroid hormone with antithyroid medications like PTU or methimazole
- Block release of thyroid hormone with inorganic iodine
- Block conversion of T4 into T3
- Block peripheral effects of thyroid hormone with beta-blockers like atenolol and [propranolol
- Block iodine uptake with the use of cholestyramine

Thank you, Good discussion