Today’s episode is dedicated to Tumor Lysis Syndrome management in the PICU. Join us as we discuss the patient case, symptoms, and treatment.
We are delighted to be joined by Dr. Himalee Sabnis, Assistant Professor of Pediatrics at Emory University School of Medicine. She is also a pediatric hematologist/oncologist and the Co-Director of the High-Risk Leukemia Team at the AFLAC Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
Show Highlights:
- Our case, symptoms, and diagnosis: A three-year-old female with pre-B ALL presents on Day 2 of chemotherapy to the PICU. She is admitted with telemetry findings of arrhythmia, decreased urine output, and an EKG notable for peaked T waves. Her labs are notable for elevated WBC, hyperkalemia, hyperphosphatemia, and low ionized calcium.
- Tumor Lysis Syndrome is a life-threatening medical emergency stemming from rapid tumor cell destruction that overwhelms the usual metabolic and excretory pathways.
- Why TLS is the most common pediatric oncologic emergency for pediatric cancer patients
- When the tumor cells die or lyse, what’s inside those cells comes out into the blood
- Key metabolic abnormalities that affect organ function are too much potassium and phosphorus, low calcium, and uric acid buildup.
- Those metabolic abnormalities can result in cardiac arrhythmia and kidney failure.
- Certain patient populations have an increased risk for TLS:
- Hematological cancers have a higher risk than solid tumors
- Patients with fast-growing tumors, like lymphoma and leukemia, are at high risk
- Key pathophysiologic principles that drive TLS:
- The imbalance of electrolytes can impact heart function
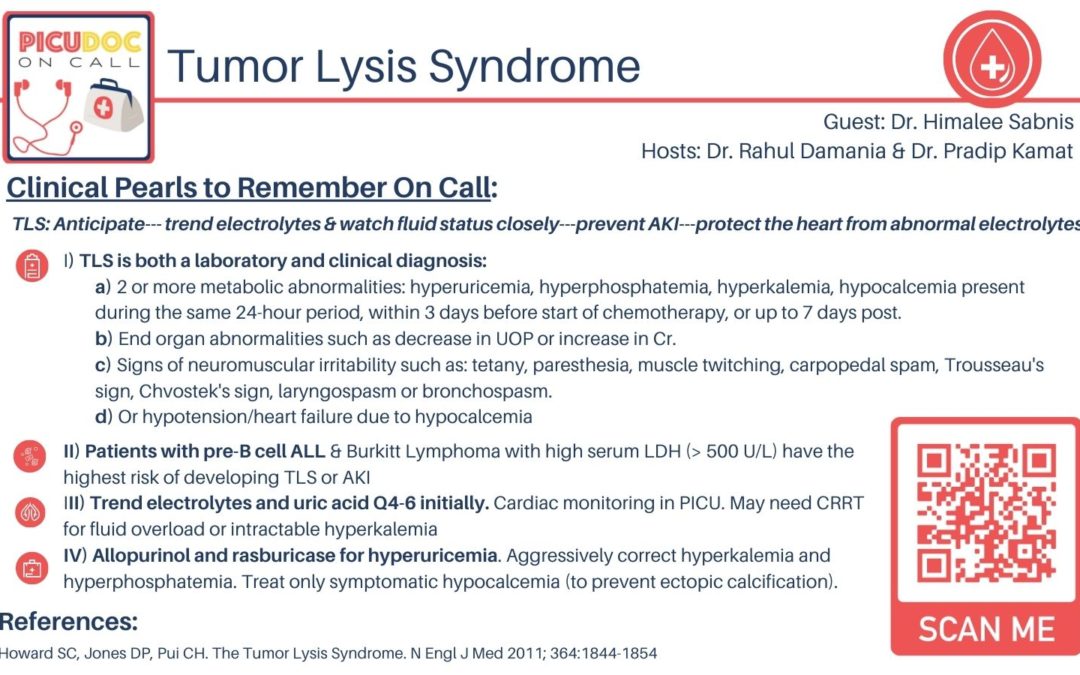
- TLS is characterized by hyperkalemia, hyperphosphatemia, hypocalcemia, and uric acid, which is a by-product of DNA breakdown
- If untreated, the uric acid can lead to acute kidney injury and renal failure
- Electrolyte and metabolic disturbances can progress to renal insufficiency, cardiac arrhythmias, seizures, and death
- TLS releases cytokines that can cause a systemic inflammatory response and multi-organ failure
- Other lab markers in patients with TLS include uric acid, LDH, CBC, DIC panel, and daily blood gas (these are typically trended every 4-6 hours).
- Key factors in TLS management are to understand the risk and know your resources.
- Steps taken would be continuous cardiac monitoring, uric acid control, administering Allopurinol to combat uric acid formation, and managing electrolyte disturbances in conjunction with an intensivist.
- Chemotherapy would not be delayed due to TLS because the patient’s condition won’t improve until the cancer is treated.
- How the complications of TLS are treated:
- Hyperphosphatemia should be treated by using oral phosphate binders such as aluminum hydroxide.
- Hypocalcemia does not require therapy unless cardiac function is affected.
- How renal replacement therapy might be required and indications are similar to other forms of acute kidney injury.
- Besides Allopurinol being given at the initiation of chemotherapy, patients at high risk for TLS may receive low-intensity initial therapy to prevent rapid cell lysis.
- Takeaway clinical pearls regarding TLS:
- Know what you’re dealing with because every cancer is different.
- Fluid management is important and will vary from patient to patient.
- Be proactive in monitoring. Intervene early and quickly.