Hosts:
- Pradip Kamat, Children’s Healthcare of Atlanta/Emory University School of Medicine
- Rahul Damania, Cleveland Clinic Children’s Hospital
Case Introduction:
- 6-year-old patient admitted to PICU with severe pneumonia complicated by pediatric Acute Respiratory Distress Syndrome (pARDS).
- Presented with respiratory distress, hypoxemia, and significant respiratory acidosis.
- Required intubation and mechanical ventilation.
- Despite initial interventions, condition remained precarious with persistent hypercapnia.
Physiology Concept: Dead Space
- Defined as the volume of air that does not participate in gas exchange.
- Consists of anatomic dead space (large airways) and physiologic dead space (alveoli).
- Physiologic dead space reflects ventilation-perfusion mismatch.
Pathological Dead Space:
- Occurs due to conditions disrupting pulmonary blood flow or ventilation.
- Common in conditions like pulmonary embolism, severe pneumonia, or ARDS.
Clinical Implications:
- Increased dead space fraction (DSF) in PARDS is a prognostic factor linked to severity and mortality.
- Elevated DSF indicates worse lung injury and inefficient gas exchange.
- DSF can be calculated using the formula: DSF = (PaCO2 – PetCO2) / PaCO2.
Practical Management:
- Optimize Mechanical Ventilation
- Enhance Perfusion
- Consider Positioning (e.g., prone positioning)
Summary of Physiology Concepts:
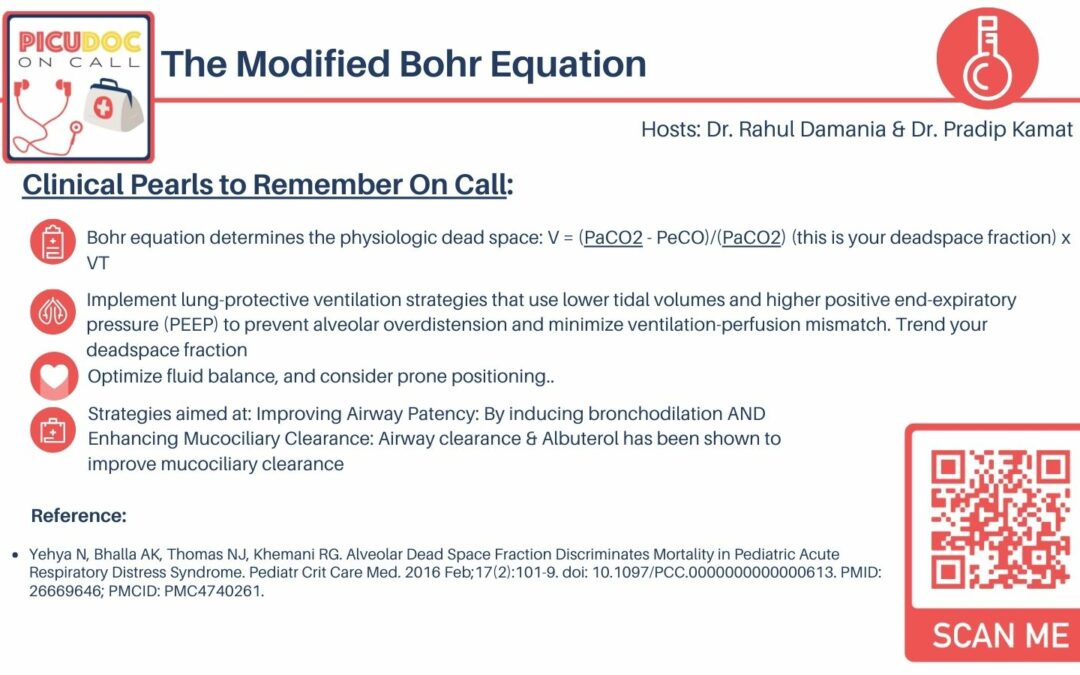
- Bohr equation for physiologic dead space.
- Importance of lung-protective ventilation strategies.
- Monitoring and trending dead space fraction.
- Strategies to improve airway patency and mucociliary clearance.
Connect with us!
- PICU Doc on Call provides concise explanations of critical concepts in pediatric intensive care.
- Feedback, subscriptions, and reviews are encouraged.
- Visit picudoconcall.org for episodes and Doc on Call infographics.
- Hosted by Dr. Pradip Kamat and Dr. Rahul Damania.
Reference:
- Yehya N, Bhalla AK, Thomas NJ, Khemani RG. Alveolar Dead Space Fraction Discriminates Mortality in Pediatric Acute Respiratory Distress Syndrome. Pediatr Crit Care Med. 2016 Feb;17(2):101-9. doi: 10.1097/PCC.0000000000000613. PMID: 26669646; PMCID: PMC4740261.