Welcome to PICU Doc On Call, A Podcast Dedicated to Current and Aspiring Intensivists.
I’m Pradip Kamat coming to you from Children’s Healthcare of Atlanta/Emory University School of Medicine. I’m Rahul Damania from Cleveland Clinic Children’s Hospital and we are two Pediatric ICU physicians passionate about all things MED-ED in the PICU. PICU Doc on Call focuses on interesting PICU cases & management in the acute care pediatric setting so let’s get into our episode.
Today, we are going to discuss the management of the postoperative patient admitted to the PICU. Our discussion will focus on the non-cardiac and non-transplant admission. Our objective in this episode is to create a framework on what areas of care to focus on when you have a patient admitted to the PICU post-operatively. Each surgery and patient is unique; however, we hope that you will garner a few pearls in this discussion so you can be proactive.
in your management. Without any further delay, let’s get started with today’s case:
We begin with a 13-year-old child, Alexa, with h/o of a genetic syndrome, who presents today with a history of thoracolumbar kyphoscoliosis. Over the years, Alexa’s curvature has progressively worsened, resulting in difficulty breathing and chronic back pain. The decision was made to proceed with a complex spinal surgery, including posterior spinal fusion and instrumentation.
In the weeks leading up to the surgery, Alexa underwent a thorough preoperative evaluation, including consultations with specialists and relevant imaging studies. Pulmonary function tests revealed a restrictive lung pattern, while the echocardiogram showed no significant cardiac abnormalities. Preoperative labs, including CBC, electrolytes, and coagulation profile, were within normal limits.
During the surgery, Alexa was closely monitored by the anesthesia team, who administered general anesthesia with endotracheal intubation. The surgery was performed by the pediatric neurosurgery and orthopedics, with intra-operative neuromonitoring to assess spinal cord function. The surgical team encountered an unexpected dural tear, which was repaired using sutures and a dural graft. Due to the prolonged surgical time, a temporary intra-operative loss of somatosensory evoked potentials was noted. However, signals were restored after adjusting the patient’s position and optimizing blood pressure. The posterior spinal fusion and instrumentation were completed successfully, but the surgery lasted 8 hours. Total intra-operative blood loss was 800 mL, and Alex received 2 units of packed red blood cells and was on NE for a little over half the case before weaning off.
Alexa was admitted to the PICU intubated and sedated for postoperative care. The initial assessment showed stable vital signs, with a systolic blood pressure of 100 mmHg, heart rate of 90 bpm, and oxygen saturation of 99% on mechanical ventilation. Postoperative pain was managed with a continuous morphine infusion. The surgical team placed a closed suction drain near the surgical site and a Foley catheter for urinary output monitoring. You are now at the bedside for OR to PICU handoff…
To summarize key components from this case:
This is a patient with thoracolumbar kyphoscoliosis, underwent complex spinal surgery (posterior spinal fusion and instrumentation) due to progressive curvature, breathing difficulties, and chronic pain.
She had a course intra-operatively, where an unexpected dural tear occurred, requiring repair with sutures and a dural graft. Temporary loss of somatosensory evoked potentials was resolved through patient repositioning and blood pressure optimization with NE.
She had a moderate amount of blood loss in the case and is back intubated, sedated, with surgical drains in place.
So Pradip, we see patients such as Alex in our PICU commonly, if we take a step back what is your general approach with children who are admitted to the PICU post operatively?
I think it’s crucial to approach the care of postoperative children in the PICU systematically and proactively. This involves closely monitoring their changing physiology, anticipating potential complications, and collaborating with the surgical team to address any concerns. By maintaining open communication and following evidence-based guidelines, we can optimize patient outcomes and facilitate a smooth recovery process.
💡
Just as a quick tid-bit, while some of these PICU admissions are scheduled, there is literature to suggest that up to 24% of non-cardiac surgeries may result in unanticipated admissions to the PICU. An single center study published in 2017 in PCCM looked at their rates of unanticipated PICU admissions from the OR, and they found that these children spend twice as much time on mechanical ventilation and that airway abnormalities, anesthetic factors, and intra-operative hypoxia contribute to such admissions.
Alright, Pradip, we are now at the post operative handoff and the first person who is going to be giving report is the anesthesia team. Can you please highlight what are some key things to listen out for during their sign out and what are some questions to ask?
Great question! The anesthesiologist plays a crucial role in ensuring the patient’s airway and hemodynamics are properly managed during surgery, which is essential for a safe and successful procedure. It’s important for the anesthesiologist to communicate with the PICU team regarding: induction, intraoperative course, line & tubes, as well as pain management.
Let’s break these down:
So for induction, you want to know were the anesthetics administered through IV or general anesthesia, was it a smooth process or were there difficulties, and what was used for anesthesia maintenance.
Next you want to know about the airway.
You want to gather essential information about the patient’s airway management. Find out if an LMA or ETT was used during the procedure. If the patient was intubated, inquire about the ease of bag-mask ventilation and laryngoscopy, as well as the grade of the glottic view (e.g., Grade 1) and the type of laryngoscope used, including if video laryngoscopy was employed. It’s also important to know the number of intubation attempts. Additionally, gather details about the type of ETT (regular or neo-cuff), its size, and the length at which it is taped to the gum or teeth. Finally, ask if any airway adjuncts were utilized during bag-mask ventilation or intubation.
🚨
Remember that a key management point as soon as handout is completed is to obtain a CXR to confirm tube placement, and work closely with your RT to secure the tube in the correct position.
That’s so true!
As you wrap up anesthesia sign out, here are some other things to think about:
Oxygenation/Ventilation: Determine if the patient was easily oxygenated and ventilated, or if any bronchospasm or laryngospasm occurred during the case.
Lines & Tubes: Inquire about IV or central access, arterial line usage, and the presence of any drains or tubes (e.g., NG, Foley).
I/Os: Understand the management of fluid, electrolyte, and glucose homeostasis during anesthetic care, including the types and rates of fluids administered, blood product usage, and estimated blood loss.
Pain Management: Gather information on the analgesics, sedatives, and neuromuscular blockers used.
Other Medications: Be aware of antibiotics, antiemetics, anticholinergics, and other medications administered during the procedure.
Duration of the Case & Patient Position: Obtain information on the duration of the surgery and the patient’s position (e.g., supine or prone, as in spinal cases).
Latest Set of Vital Signs: Ensure you have the most recent vital signs recorded.
⚖️
A nice mnemonic that I use is:
A – Airway: LMA/ETT, ease of ventilation, glottic view, laryngoscope type
P – Pain Management: Analgesics, sedatives, neuromuscular blockers
I – I/Os: Fluids, blood products, estimated blood loss
L – Lines & Tubes: IV/central access, arterial line, drains, NG, Foley
O – Oxygenation/Ventilation: Oxygenation ease, bronchospasm, laryngospasm
T – Time & Position: Duration of case, patient position (supine or prone)
Especially when it comes to access, coordinating with your PICC team, surgery colleagues, or anesthesia teams of long term access or additional PIVs which can be placed while the patient is under anesthesia is key!
Absolutely, Rahul! It’s important for us to also recognize that general anesthesia can cause vasodilation, and when combined with surgical blood loss and insensible losses, it increases the need for fluids postoperatively. Factors like prone positioning and mechanical ventilation can also affect urine output, making it a less reliable indicator of intravascular volume. In the postoperative period, it’s important to administer isotonic fluids to avoid hyponatremia and watch for SIADH. Additionally, since operating rooms can be cold, it’s crucial to monitor the patient’s temperature, especially in infants, to prevent complications like arrhythmias and coagulation disturbances due to hypothermia.
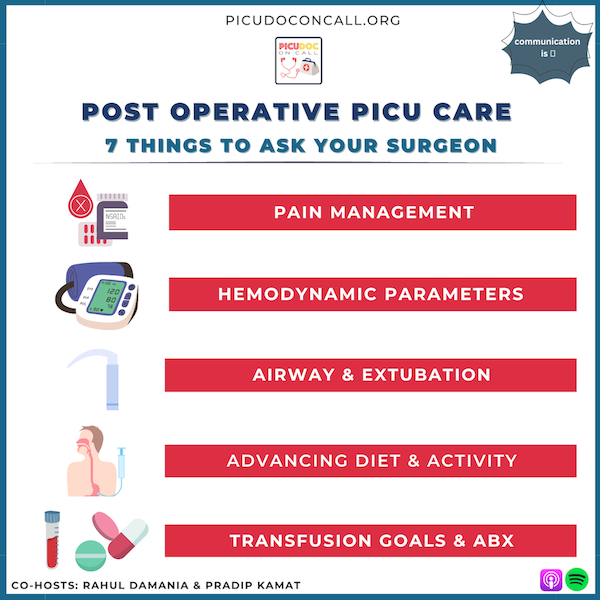
Let’s transition, Pradip. When admitting a postoperative patient to the PICU, what essential questions should we ask the surgeons?
As we have our patient post-op in the PICU, we need to have a clear understanding of the type of surgery performed. Additionally, we should ask these key questions to ensure comprehensive patient management. Communication is essential!
We have arranged this into organ systems, and while not all of these questions would be applicable to every case, this list is relatively comprehensive!
Let’s start with our first organ system:
CNS:
What are the acceptable pain management medications for the immediate post-op period? Can we consider PCA, non-opioids like ketorolac or other NSAIDs, or IV acetaminophen?
Are there any activity restrictions for the patient, or can they be mobilized early? When can we involve PT/OT and speech therapy in the patient’s care?
Respiratory:
2) If the patient is admitted to the PICU intubated, when can they be extubated?
If extubation is unsuccessful, can non-invasive positive pressure ventilation, such as HFNC or BiPAP, be used? This is especially true for intra-abdominal procedures.
Is perioperative dexamethasone appropriate?
Are there any procedures like MRI or a revisit to the operating room needed prior to extubation?
⚖️
Just to loop back to a prior concept which we discussed, you want to know if the patient at minimum can be bag masked, was the airway difficult, if there is an acute airway event should the PICU team be the primary team to intubate or should this be an intubation by Anesthesia or ENT.
Cardiovascular:
3) What are the target blood pressure goals (systolic or MAP) for the patient postoperatively?
This will be especially true for neurosurgical procedures and even transplant patients.
⚖️
If you have yet to check them out, please consider listening to our prior episodes on the post operative approach to Renal transplant and Liver tranplant in the PICU!
Fluid, Electrolytes, and Nutrition/GI:
4) When can the patient begin clear fluids and advance their diet?
Renal:
5) Can the Foley catheter be discontinued, and if so, when?
Talk about urine output goals when applicable.
⚖️
Also note that another output which you may have to keep in mind will be how much drainage will be coming out of your peritoneal, penrose, CSF drain — clarifying thresholds of quality and quantity of drainage with your surgical teams can really help with effective recognition of post operative complications. Coordinating a plan to replace the excessive out fluid and with type of fluid is key?
Hematology:
6) Which labs (such as CBC, electrolytes, or coagulation profile) need to be obtained, and how frequently?
Are there any specific transfusion goals?
Infectious Diseases:
7) What antibiotics are prescribed, and for what duration? If the patient becomes febrile, should cultures be obtained?
⚖️
Alright summary, analgesia, airway, BP goals, diet/activity, transfusion thresholds, antibiotics & repeat imaging.
Rahul, there seem to be several logistical questions to consider as well. Could you please highlight the key aspects for us?
Certainly, it’s crucial to address logistical factors in postoperative care. Firstly, we need to determine when a patient, who is extubated and on room air and hemodynamically stable, can be transferred out, especially if bed capacity is limited. Secondly, it’s essential to verify whether the child’s family or guardians have been updated on their condition. Lastly, we should inquire about any additional consults that need to be placed for the PICU team to ensure comprehensive patient care.
We want to conclude this episode by delving deep into a few of the patients which are commonly admitted to the PICU post operatively. Our goal here is to apply the principles of management we just learned.
The first case we want to return to is our post-operative spinal fusion.
How does their pre-op status influence the post-op course?
The post-op course depends on pre-op status, pulmonary function, degree of curvature, and extent of repair. Key concerns include paralysis, pain management, airway maintenance, and pulmonary hygiene.
⚖️
The key here is to work closely with your pulmonary colleagues and RT to coordinate an effective bronchopulmonary hygiene regimen while admitted in the hospital as effective airway clearance can optimize cardiorespiratory status.
What complications should we watch for due to spinal cord manipulation?
Watch for SIADH and check sodium levels if urine output decreases. A high heart rate might be due to pain, so check intra-operative records for more information.
Alright our next Rapid Fire Case: ENT or OMFS procedures like tracheostomy, TNA, SGP, and airway reconstruction!
What should we know about post-op management for typical ENT procedures like tracheostomy or airway reconstruction?
Get information on bag-mask ventilation and intubation options in case of unplanned extubation. Check if NIPPV is contraindicated. Be prepared for blood loss, post-op swelling, and airway emergencies with wire cutters and spare tracheostomy.
How should we handle a dislodged tracheostomy in a fresh case?
Consult the ENT surgeon for a fresh tracheostomy dislodgment. Forcing a trach can create a false track. Some trachs have stay sutures for guidance. Difficult airway patients may need deep sedation or paralysis until the first tracheostomy change.
💡
In airway emergencies it is vital to remember that what the patient requires is oxygen and not a device. So instead of trying to force a device say through a tracheostomy etc-the patient should be given 100% oxygen via bag-mask ventilation while appropriate help is summoned.
Alright, our final rapid review case are neurosurgical procedures such as craniosynostosis repairs, disconnective hemispherectomies, and drain placements.
What should we consider, in general, for post-op management of neurosurgery patients?
Be prepared for large blood loss and fluid replacement during surgery. Monitor fluid status, blood loss, pain management, and closely observe neuro-monitoring in the PICU. Watch for facial and scalp swelling as this may play into airway plans. Also, Keep a close eye on the amount of CSF drained, potentially replacing the CSF if needed. Monitor serum sodium carefully since CSF is rich in sodium.
This is great, I do also want to highlight any trauma or intra abdominal procedures that may be admitted into the PICU. It’s important to focus on judicious management of pain, fluids, and electrolytes, while staying vigilant for infection, urine output, abdominal distension, and acute kidney injury. Monitor for complications like ARDS, TRALI, and TACO, especially if massive transfusion protocol was used prior to or during surgery. Working closely with surgeons regarding return to bowel function and nutrition is also essential!
We talked about some very important management points today, can you do a quick summary?
Know anesthesia details: induction method, airway management, medications used, and complications encountered.
Ask key post-op questions: pain management, activity restrictions, airway concerns, transfusion goals, and antibiotic usage.
Understand post-op management for specific surgeries: spinal fusions, ENT procedures, and neurosurgical cases; monitor for complications and work closely with surgical teams.
Remember, fostering open dialogue and collaboration between the multidisciplinary PICU team, surgical teams, and families to ensure comprehensive post-op care can help prompt the best possible outcomes for each patient. Having a structured handoff technique has been shown to also help enhance communication. Together, we can make a difference in the lives of our young patients!
This concludes our episode on the operative child in the PICU We hope you found value in our short, case-based podcast. We welcome you to share your feedback, subscribe & place a review on our podcast! Please visit our website picudoconcall.org which showcases our episodes as well as our Doc on Call management cards. PICU Doc on Call is co-hosted by myself Dr. Pradip Kamat and Dr. Rahul Damania. Stay tuned for our next episode! Thank you!
References
Fuhrman & Zimmerman – Textbook of Pediatric Critical Care Chapter Section XIV.Pediatric Critical Care: Anesthesia Principles in the Pediatric Intensive Care Unit: Page 1509-1628. Chapters 127-135
Sochet AA, Siems A, Ye G, Godiwala N, Hebert L, Corriveau C. Standardization of Postoperative Transitions of Care to the Pediatric Intensive Care Unit Enhances Efficiency and Handover Comprehensiveness. Pediatr Qual Saf. 2016 Nov 29;1(2):e004. doi: 10.1097/pq9.0000000000000004. PMID: 30229145; PMCID: PMC6132582.
Quinn TD%2C Gabriel RA%2C Dutton RP%2C Urman RD. Analysis of Unplanned Postoperative Admissions to the Intensive Care Unit. J Intensive Care Med. 2017 Aug%3B32(7)%3A436-443. doi%3A 10.1177/0885066615622124. Epub 2015 Dec 30. PMID%3A 26721638.
Mitchell J, Clément de Clety S, Collard E, De Kock M, Detaille T, Houtekie L, Jadin L, Bairy L, Veyckemans F. Unplanned intensive care unit admission after general anaesthesia in children: A single centre retrospective analysis. Anaesth Crit Care Pain Med. 2016 Jun;35(3):203-8. doi: 10.1016/j.accpm.2015.10.005. Epub 2016 Jan 19. PMID: 26804922.

Great review thank you! I also was interested in your thoughts about post op cases of 8 hours 16 y/o spinal fusion for cervical to lumbar scoliosis repair- dealing with all the hemodymatic issues because of 6 l N.A. / 2 L LR 1 unit pencil albumin cell saver used to prevent additional blood loss- to me best care would be patient goes directly to ICU not pediatric unit with one nurse on a 5 or 6 patient assignment if only for pain management not to mention the issue of hemodymatics. Any comment would be appreciated thank u!