Welcome to PICU Doc On Call, A Podcast Dedicated to Current and Aspiring Intensivists.
I’m Pradip Kamat and I’m Rahul Damania. We are coming to you from Children’s Healthcare of Atlanta – Emory University School of Medicine.
Welcome to our Episode a 2-year-old with severe pallor and O2 desaturation.
Here’s the case presented by Rahul:
A two-year-old presents to the PICU with severe pallor + O2 requirement. The patient went for a routine check with her primary care who noted the patient appeared severely pale. He sent the patient to the ED. An initial Hgb check revealed a Hgb of 1.5gm/dL. Per mother, she is otherwise healthy but a very picky eater. She also reports the patient drinks milk as a soothing adjunct at night, consuming between 12 – 36oz a day. No family h/o of anemia or any other blood disorders.
No h/o recent illness. Mother had a normal spontaneous full-term delivery. The patient is up to date on her immunizations. Per mother, developmental milestones are normal. The mother also denies any history of decreased activity in the child. Given the low Hgb, the patient was admitted to the PICU.
Let’s transition into some history and physical exam components of this case?
What are key history features in this child?
- Severe pallor in a 2-year-old
- H/o being a picky eater
- H/o excessive milk consumption
- Pertinent negatives include: No obvious blood loss, No petechia, bruising, or jaundice
What did the physical exam show?
- The patient was hypertensive, tachycardic to the 140s, and 10th% weight for growth percentiles
- On physical exam, the patient was in no acute distress. Her lips, gums, and conjunctiva were pale. She had a systolic ejection murmur. As a pertinent negative, she had no hepatosplenomegaly. She also has no rash, bruising, or petechiae.
The lack of hepatosplenomegaly may indicate that the patient has no signs of extramedullary hematopoiesis. Patients with hemolytic processes resulting in anemia may present with signs of scleral icterus, jaundice, and hepatosplenomegaly resulting from increased red cell destruction. In fact, in an emergency department setting, the clinical detection of jaundice was found to have sensitivity and specificity of only approximately 70 percent.
To continue with our case, then what were the patient’s labs consistent with:
- Initial CBC showed: WBC 8.5K, RBC 1.14 (L), Hgb 1.5gm/dL; Hct 6.1, MCV 53.5, and an elevated RDW 37.7. Initial platelet count was 50K, reticulocyte count 1.1%
- Peripheral smear revealed no blasts, thrombocytopenia – with occasional medium-sized platelets – ghost cells and anisocytosis/poikilocytosis- which appears most consistent with iron deficiency.
- It was interesting that the patient had thrombocytopenia
Absolutely, typically with Iron deficiency, there is thrombocytosis (erythropoietin is increased which closely mimics thrombopoietin stimulates platelets). In fact, both act via the non-TK, JAK-STAT pathway.
OK, to summarize, we have:
- Two year old with severe anemia most likely secondary to iron deficiency.
- As you think about our case, what would be your differential?
- For any patient with acute severe anemia presenting to the PICU- One has to think in terms of blood loss, decreased or impaired production (i.e bone marrow failure), or peripheral blood destruction (i.e hemolysis).
- Here would be the organizations:
- Blood loss
- Decreased or impaired production
- Increased destruction
Let’s go into detail for each:
- Blood loss can be internal or external (due to trauma, excessive blood draws, due to surgery)-typically gives rise to normochromic normocytic anemia.
- Decreased or impaired production: Deficiency of substances needed for Hgb & RBC production such as iron Vit B12 etc. Depression of BM due to infection (parvo B), chemicals, pharmacologic agents or immune mechanisms. Bone marrow aplasia can be idiopathic with or without congenital anomalies. Infiltration of BM due to malignancies such as leukemia, Hodgkin disease, neuroblastoma, etc.
Increased blood destruction:
- Can be due to intrinsic defects of the RBC such as hereditary spherocytosis, defects of Hgb such as sickle cell disease, thalassemia syndromes, enzyme defects.
- Extrinsic factors include immune mechanisms which can be related to drugs, infections, and non-immune mechanisms such as drugs, toxins, sepsis, HUS, TTP.
- Also a combination of intrinsic and extrinsic defects such as PNH, Favism, G-6PD. Patients with peripheral destruction in addition to pallor, typically have evidence of hemolysis such as jaundice, red cell breakdown (erythrocyte fragmentation) on the peripheral smear is seen typically in microangiopathic hemolytic anemias.
- There is typically an increase in the reticulocyte count, which keeps the MCV in the macrocytic range. Bone marrow will typically reveal erythroid hyperplasia. The sine qua non of immune hemolysis is the demonstration of the presence of antibodies or complement components bound to the erythrocyte membrane using the Direct Coombs test.
A prospective study by Bateman ST et al (Am J Respir Crit Care Med. 178:26-33 2008) reported 73% of blood loss in the PICU is attributable to blood draws. We need to limit both the number as well as the frequency of blood tests in our patients especially if these are not helping make a change in patient management. Conservative blood draws will help reduce blood transfusions in patients in the PICU. The SCCM’s “Choose Wisely” campaign recommendations from 2015 advises us not to order diagnostic tests at regular intervals (such as every day) but rather in response to specific clinical questions.
Rahul, can you give us a brief synopsis on the physiology of iron metabolism in the human body?
- Iron metabolism is unique in that iron balance is achieved by control of absorption rather than by excretion.
- About 1.5mg/day of iron is lost due to cell exfoliation from the skin, gut, and urinary tract.
- About twice this amount is lost by menstruating women and about three one-half times lost during pregnancy.
- Dietary iron is either in form of heme iron (from hemoglobin and myoglobin of animal sources) or non-heme iron from salts of non-animal sources. The mucosal cell of the small intestine (mostly duodenum and ileum) ultimately controls the absorption of iron in the body. Once taken up by the mucosal cell the iron is either incorporated into the ferritin of the mucosal cell (sloughed off in 3-4 days) or transferred to the portal circulation of the liver with help of mucosal cell transferrin.
The cellular metabolism of iron is mediated by three proteins:
- Transferrin, transferrin receptor, and ferritin.
- Transferrin production is increased in iron deficiency states. Iron storage exists in the soluble easily available form ferritin or insoluble more stable fraction hemosiderin. Ferritin is widely distributed in all cells whereas hemosiderin is deposited primarily in the liver, spleen, and bone marrow. Serum ferritin < 10 or 12 microgm/ml indicated depletion of iron reserves.
To summarize, iron metabolism uptake occurs primarily in the duodenum. Thus, always watch out for patients with duodenal disease, for example, short gut, celiac, IBD, etc. Also, transferrin transports iron, and ferritin represents your stores
Rahul, a frequently asked question on the Peds CCM boards is about oxygen content and oxygen delivery. Can you shed some light on this with the respect to this case?
We have discussed this in detail in episode 33: Oxygen Content and Oxygen Delivery. Definitely worth a listen.
- As a review, the formula for O2 content is 1.34 X Hgb X O2 saturation +0.003X PaO2.
- If we assume PaO2 is 100 and O2 saturation is 100%, our O2 content for this patient = (1.34 X 1.5 X 1) +0.003 X 100 = 2.01+ 0.3 = 2.31 ml O2/dL
- If patient is transfused to a Hgb of 6, O2 content = 8.04+0.3 = 8.34
- Conversely, If patient is given 100% O2, the PaO2 = 713, The O2 content of above patient is 2.10+ 0.003 X 713 =4.239,
- So we either have to increase the Hgb or if unable to transfuse, increase PaO2 as shown in the calculations above.
- What gives us more bang for our buck is increasing Hgb concentration — this will in turn increase our O2 content.
I think it is great to practice calculations of the O2 content, anytime they are faced with a patient with low Hgb or a patient for whom blood transfusion on is indicated. I would also recommend folks read the TAXI guidelines for pRBC transfusion in the Peds ICU. (PCCM)
If you had to work up this patient with severe anemia, what would be your diagnostic approach?
- CBC with differential, reticulocyte count, peripheral smear
- CMP, urine analysis, stool guaiac
- Infectious workup should include RVP, Parvovirus
- Hgb electrophoresis
- Serum lead level
- If the patient has pancytopenia despite PRBC replacement, she would need workup for bone marrow arrest/failure process – such as peripheral flow, BMA/Bx
- No single test or combination of tests reliably documents iron deficiency in all clinical situations. I would also add that review of the peripheral smear is an essential part of any anemia evaluation. Even if the patient’s RBC indices are normal, a review of the blood smear may reveal abnormal cells that can help identify the cause of anemia.
- If our history, physical, and diagnostic investigation led us to severe most likely due to iron deficiency anemia as our diagnosis what would be your general management of framework?
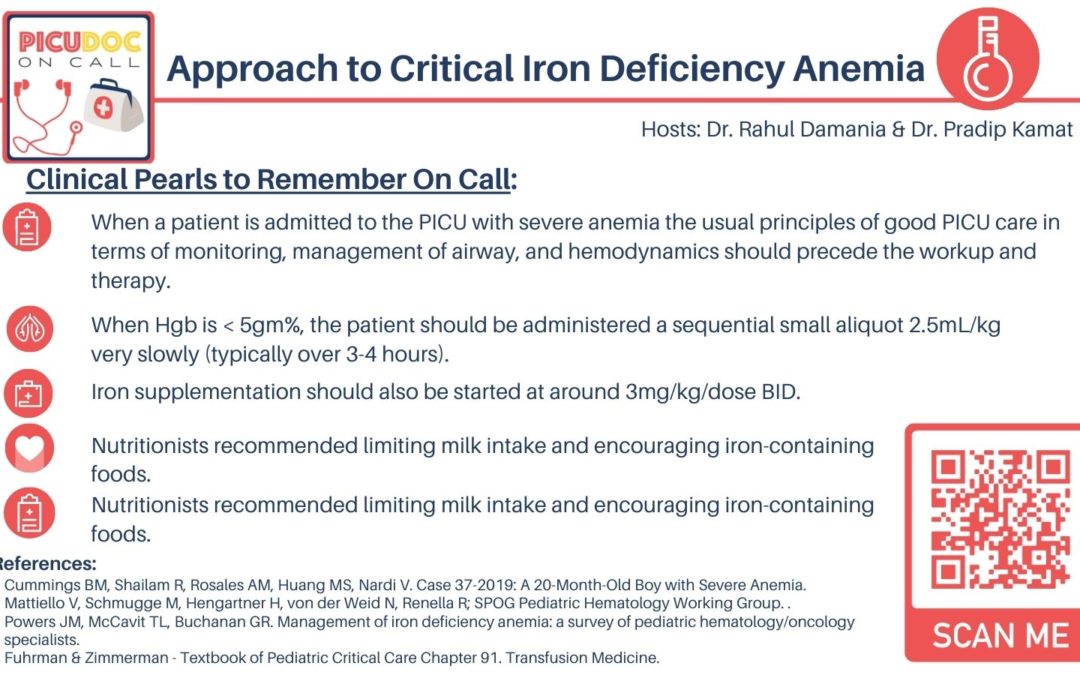
- When a patient is admitted to the PICU with severe anemia the usual principles of good PICU care in terms of monitoring, management of airway, and hemodynamics should precede the workup and therapy. I also make sure the patient has at least two good peripheral IVs of which one can be used to send the required labs. We work very closely with our hematology colleagues and the nutritionist.
- When Hgb is < 5gm%, the patient should be administered a sequential small aliquot 2.5mL/kg very slowly (typically over 3-4 hours). Frequent rechecking of hgb/hct is required as well as close monitoring for any signs of heart failure. Once Hgb is > =5gm%, we can give 5ml/kg over 2-3 hours and wait at least 2 hours in between aliquots.
- Absolutely, Rahul, Iron supplementation should also be started at around 3mg/kg/dose BID.
- Nutritionists recommended limiting milk intake and encouraging iron-containing foods and eating a healthy toddler diet. iron should not be taken with Calcium but Vitamin C, which promotes its absorption.
- Social work referral to get family the necessary support may be needed. Especially if there is a concern for lead in the home.
It is also essential to involve the Pediatric Hematology team for appropriate workup, management and follow-up!
This concludes our episode on acute anemia in the PICU. We hope you found value in our short, case-based podcast. We welcome you to share your feedback, subscribe & place a review on our podcast! Please visit our website picudoconcall.org which showcases our episodes as well as our Doc on Call management cards. If you are interested in learning more regarding acute severe anemia please refer to Fuhrman & Zimmerman – Textbook of Pediatric Critical Care Chapter 91. Transfusion Medicine. PICU Doc on Call is co-hosted by myself Dr. Pradip Kamat and Dr. Rahul Damania. Stay tuned for our next episode! Thank you!
- Cummings BM, Shailam R, Rosales AM, Huang MS, Nardi V. Case 37-2019: A 20-Month-Old Boy with Severe Anemia. N Engl J Med. 2019 Nov 28;381(22):2158-2167. doi: 10.1056/NEJMcpc1904048. PMID: 31774963
- Mattiello V, Schmugge M, Hengartner H, von der Weid N, Renella R; SPOG Pediatric Hematology Working Group. Diagnosis and management of iron deficiency in children with or without anemia: consensus recommendations of the SPOG Pediatric Hematology Working Group. Eur J Pediatr. 2020 Apr;179(4):527-545. doi: 10.1007/s00431-020-03597-5. Epub 2020 Feb 4. PMID: 32020331.
- Powers JM, McCavit TL, Buchanan GR. Management of iron deficiency anemia: a survey of pediatric hematology/oncology specialists. Pediatr Blood Cancer. 2015 May;62(5):842-6. doi: 10.1002/pbc.25433. Epub 2015 Feb 7. PMID: 25663613; PMCID: PMC4376588.
- Fuhrman & Zimmerman – Textbook of Pediatric Critical Care Chapter 91. Transfusion Medicine.