Welcome to PICU Doc On Call, A Podcast Dedicated to Current and Aspiring Intensivists.
I’m Pradip Kamat and I’m Rahul Damania. We are coming to you from Children’s Healthcare of Atlanta – Emory University School of Medicine.
Welcome to our Episode of 17-year old with h/o of SLE and now acute liver failure.
Here’s the case presented by Rahul:
A 17-year old teenage female year old presents to the PICU with acute liver failure. Important past h/o includes a diagnosis of SLE on therapy with prednisone, mycophenolate (cellcept), and plaquenil.
4 days prior to this admission, patient presented to an OSH with RUQ pain, vomiting (non bloody & no bilious), fever & malaise. Initially due to concern for “lupus Flare” patient was given steroids at the OSH.
At the OSH notable initial labs included a mild transaminitis and an INR of 1.5. She suddenly at the OSH developed fluid refractory hypotension and was started on a pressor. Due to continued worsening of her transaminitis well as a rising INR on her repeat labs she was referred to our tertiary PICU for further management.
Pertinent history also includes a negative urine pregnancy test. No recreational drug use, and only as needed use of Tylenol.
She now is in the PICU. She generally appears tired and ill. She is tachypneic on 4 LPM of nasal canulla and her oxygen saturation is 98%. She has a non-focal lung exam.
Her cardiac exam is notable for tachycardia, and pertinently no gallop, rub or murmur.
Her abdominal exam is non-focal except for mild discomfort on palpation of the RUQ with a palpable liver edge. Her extremities are cool with 3-4 capillary refill time. She is able to answer questions but intermittently doses off. No rash is noted.
To summarize key elements from this case, this patient has:
- H/o of lupus and is on immunosuppressive medications
- New onset fever/malaise
- This sounds like a LUPUS flare as she has a clinical picture of generalized inflammation.
Rahul: Lets pause right here and take a look at key history and physical exam components in a patient who has a chronic auto-immune condition:
- Fever, malaise and feeling tired all signs of constitutional symptoms.
- She has abdominal pain and vomiting that could again be related to systemic inflammation but also an intra-hepatic lesion.
Are there some red-flag symptoms or physical exam components which you could highlight?
- This patient has signs of shock!
- Tachycardia with delayed cap refill and cool extremities
- Tachypnea
- & hepatomegaly which could indicate increased central venous pressures.
- Initially her outside presentation of fluid refractory shock is of utmost concern!
- Fluid refractory shock with multi organ presentation involving liver, kidney and the blood/coagulation systems
- All of these elements bring up a concern for some acute life threatening process such as sepsis, or even immune dys-regulation due to her h/o of Lupus
- To continue with our case, the patients labs were consistent with:Acute liver dysfunction (Elevated AST and ALT in the thousands, Total bilirubin 1.6, GGT 56) although the total bilirubin is not elevated to a degree I would expect.
- AKI (creatinine 2.18)
- An uptrending Coagulopathy with elevated PT and INR: PT 120 and a peak INR of 16
- Thrombocytopenia: Platelets < 50K
- She had a peak lactate 9.2
- and concurrent Metabolic acidemia: serum HCO3 7, and pH 7.18.
- A Pertinent negative: Normal serum ammonia <38 micromol/L (nl < 50)
- Finally, she had an elevated WBC 20.5K/ Hgb 9.7, Platelet 42. CRP 4.2/ESR 5
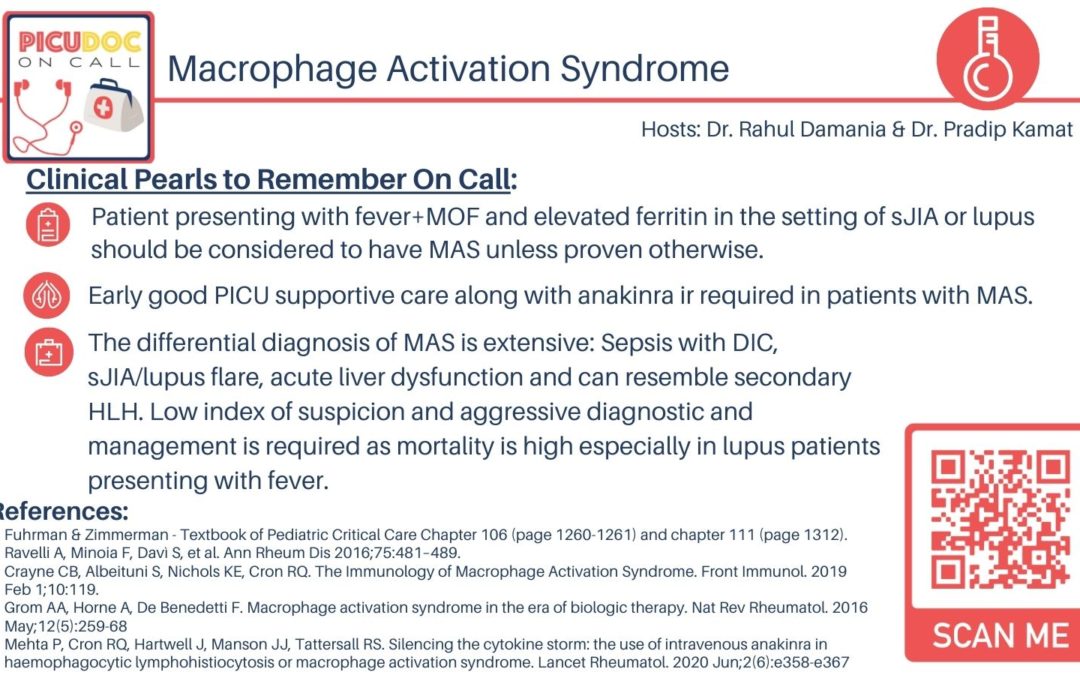
OK to summarize, we have: a 17 yr old female with SLE on mycophenolate (cellcept) who presents with fever, hypotension, AKI and liver dysfunction with severe coagulopathy, although we do not have other labs- This brings up the concern for acute macrophage activation syndrome (MAS) the topic of our discussion today.
- Let’s start with a short multiple choice question:
- 12 year old male with h/o systemic onset juvenile idiopathic arthritis (JIA) presents with fever, rash, hypotension, acute respiratory distress with hypoxia. Mental status is normal. He also has acute kidney injury, transaminitis, coagulopathy, metabolic acidemia as well as anemia and thrombocytopenia. His liver and spleen are enlarged and he has scattered lymphadenopathy. The laboratory findings most suggestive of acute macrophage activation syndrome in this patient is:
- Erythrocyte Sedimentation Rate > 100
- ADAMS13 activity < 10%
- Serum Ferritin > 20, 000ng/mL
- Fibrinogen (> 500mg/dL)
- The correct answer is serum ferritin > 20,000ng/mL. Any patient with systemic JIA who presents with high fever, heptao-splenomegaly with evidence of multi-organ dysfunction should be considered to have the potentially life threatening complication of systemic inflammatory disorders: acute macrophage activation syndrome (MAS) unless proven otherwise. The 2016 Classification criteria for MAS was published (Ravelli A. et al. Ann Rheum Dis 2016; 75:481-489) requires a Ferritin > 684ng/mL and any two of the following:
- A platelet count < 181 X 109/L (181K)
- AST > 48units
- Triglycerides > 156 mg/dL
- Fibrinogen ≤ 360mg/dL
OK lets summarize, platelets less than 180K, fibronogen <360, transaminitis >AST 48 and hypertriglcyeridemia! Remember many of these values are acute phase reactants
Correct Rahul, also the above Laboratory abnormalities should not be otherwise explained by another patient condition, such as concomitant immune-mediated thrombocytopenia, infectious hepatitis, visceral leishmaniasis or familial hyperlipidemia.
Are there any other inflammatory mediators or subtleties you would like to highlight with this disease?
- A falling ESR, especially with a high CRP, is concerning for MAS and is secondary to low fibrinogen in the setting of consumptive coagulopathy.
- In the question, patient’s ESR is elevated. Low or absent ADAMS T-13 activity is more suggestive of thrombocytopenic purpura (TTP), which is not the case here as mental status is preserved indicating no CNS involvement. In MAS there is typically consumption of fibrinogen not its elevation. The elevated ferritin (> 10,000ng/mL) along with other systemic findings in the patient in the question is highly suggestive of MAS. Additional labs that would suggest MAS include demonstration of hemophagocytosis in bone marrow or other tissue, elevated D-dimers, lactic acid dehydrogenase (LDH), triglycerides, low natural killer (NK) cell function, and elevated soluble IL-2 receptor levels.
Great highlight of the incorrect answers the pathophysiology of increased immune activation is key along with dysfibrinogenemia — this is likely due to microangiopathic consumption
Rahul can you briefly tell us a bit about macrophage activation syndrome?
- MAS is classified among the group of hemophagocytic lymphohistiocytosis (HLH), so HLH is the umbrella term.
- HLH includes familial HLH and secondary HLH. Secondary HLH is triggered by several causes, including infection, drugs, malignancy, and rheumatic disorder. Remember in our case the patient had Lupus
- In MAS A common hypothesis in MAS is that there is a defect in lymphocyte cytolytic activity, which means that lymphocytes are not able to kill cells appropriately.
Let’s break down the pathophysiology a bit further.
- There is a genetic predisposition, and that is to having increased macrophage responsiveness
- There is some form of background inflammatory activity. What cytokines are elevated?
- IL-6
- IL-1
- IL-18
- What does IL-6 do?
- Decreases NK cell function
- So now you have bad T cell cytolytic function and decreased NK cell cytolytic function. What does this lead to?
- Prolonged cell to cell interactions and amplification of a pro0inflammatory cascade.
- So now we have genetic predisposition some background cytokine inflammatory activity with cytokine production and now we layer in the third element of the pathophysiology — A trigger!
- What are triggers: acute on chronic inflammation & especially infection!
- This trigger will be important to capture in our understand as management will be geared towards reversing this trigger. So where does the hemophagocytosis come about in the term hemophagocytic lymphohistiocytosis? Well, the cytokine storm results in activation of macrophages which are known as hemophagocytes. There’s a particular cytokine IFN gamma that make macrophages angry and it is this response that can lead to multi-organ dysfunction.
Pradip, now with this summary let’s dive into MAS and how it relates to HLH?
- MAS is a life threatening illness is a form of secondary hemophagocytic lymphohistiocytosis (HLH) and a common complication of rheumatologic conditions, such as systemic JIA. The occurence of MAS has been well reported in other autoimmune or auto-inflammatory conditions, such as, adult-onset and childhood-onset systemic lupus erythematosus, Kawasaki disease, and periodic fever syndromes.
- Characteristic clinical features of MAS are high, non-remitting fever, hepatosplenomegaly, generalized lymphadenopathy, central nervous system dysfunction and hemorrhagic manifestations.
- Typical laboratory abnormalities include pancytopenia, increased levels of ferritin, liver enzymes, lactate dehydrogenase, triglycerides, D-dimers and soluble interleukin 2 (IL-2) receptor α (also known as soluble CD25 (sCD25)), and decreased fibrinogen levels.
- A typical histopathological feature of MAS is the accumulation of well differentiated macrophages exhibiting hemophagocytic activity in bone marrow biopsy specimens or aspirates. Although the prevalence of MAS among patients with systemic JIA has been estimated to be ∼10%, recent reports suggest that subclinical MAS may occur in as many as 30–40% of patients with systemic JIA.
- MAS can result in progressive multiorgan failure and eventually a fatal outcome if unrecognized. Recent studies indicate a mortality rate of 8%. Early recognition of MAS is often challenging, given the lack of a single pathognomonic clinical or laboratory feature. Furthermore, histopathological features of hemophagocytosis may not be present in the initial stages and lack specificity for hemophagocytic syndromes. In addition, features of MAS may be difficult to distinguish from other conditions that may present with overlapping manifestations, such as flares of systemic JIA, lupus or systemic infections.
- MAS associated with SLE is rare and the incidence is about 0.9–4.6% but survival from MAS in febrile SLE patients who are admitted to the hospital ranges is 64% vs 97%.(p<0.001) in those without MAS. The odds of in-hospital mortality was 64.5, 95% CI: 7.6-544; p<0.001).
OK so HLH is the umbrella term and if a patient has signs and symptoms of acute inflammation + end organ dysfunction with a chronic rheumatological disease, you defintiely want to consider MAS. MAS in febrile SLE patients has a poor outcome.
As you think about our case, what would be your differential?
- Sepsis with DIC or liver dysfunction
- Flare of systemic JIA, lupus or primary rheumatologic disease
- Remember cytokine release syndrome in patients who get CAR-T therapy is a form of MAS.
Pradip: If you had to work up this patient with MAS what would be your diagnostic approach?
Initial labs include: CBC with diff, DIC panel, CMP, Ferritin, Soluble IL-2R. Blood/urine analysis/cultures. Patient in MOF, I would also trend lactates, blood gas, CMP and DIC panel at least every Q12 and as needed. Consult with rheumatology, infectious disease experts for their help with diagnosis and management. Given difficulty with distinguishing acute liver failure with DIC from MAS, factor V, VII and VIII levels (decreased in sepsis but not in liver disease) may be helpful. Additionally, PICU docs must be vigilant for neutropenic sepsis and opportunistic fungal infections, correct electrolyte imbalances, and use blood products to correct anemia, thrombocytopenia and coagulopathy.
- Alternative biomarkers for MAS—such as soluble IL-2 receptor, CD163, and IL-18—have shown promise. However, these tests are not universally available and generally have long turnaround times.
- It is important to r/o infection early but that may be difficult to do. I would send a viral panel which includes SARS COV-2 PCR
- Imaging: CXR, abdominal ultrasound, and echocardiography
Ferritin > 10K with evidence of hemophagocytosis in the bone marrow is most suggestive of MAS in a patient who has a presentation suggestive of MAS.
Pradip: If our history, physical, and diagnostic investigation led us to Macrophage activation syndrome (MAS) as our diagnosis what would be your general management of framework?
- Good basic PICU care with close attention to airway, breathing and hemodynamics. As modern medicine is a team sport consult with ID, rheumatology, hepatology etc. These patients typically need mechanical ventilation (On CMV use a high PEEP, low FIO2, low TV lung protective strategies). Patients may need HFOV for pulmonary hemorrhage. CVL, arterial lines should be placed. Avoid benzodiazepines for sedation, and prevent secondary kidney or liver toxicity (avoid nephrotoxic medications, dose antibiotics based on levels, avoid acetaminophen). As MAS is not readily distinguishable from sepsis-initial broad-spectrum antibiotics should be initiated.
- Although previously steroids/cyclosporine were the first line therapy: More recently, cytokine specific therapy with agents like anakinra an IL-1 receptor antagonist (2-4mg/kg s.c. every 6-24 hours) is rapidly effective. Anakinra blocks the biologic activity of both IL-1α and IL-1β by competitively inhibiting their binding to IL-1R. IV anakinra may be indicated if platelets < 20, neurologic symptoms and subcutaneous skin edema. A distinct advantage of anakinra is that the drug is less hepatotoxic, less immunosuppressive and has shorter half-life compared to etoposide or tocilizumab. Anakinra may help avoid steroids especially if diagnosis is not clear and there is a danger of masking lymphoma due to the steroids.
- Rahul its important to note that 2 other drugs (IL-1 beta receptor antagonist canakinumab and IL-6 inhibitor tocilizumab) while decreasing some of the clinical findings of MAS- such that patients may present with less fevers and hepatomegaly, as well as change lab features and the patient can thus have lower ferritin, lower fibrinogen, and lower CRP. Moreover, the excellent response of sJIA features to canakinumab and tocilizumab with simultaneous development of MAS features in some patients also suggests that the role of IL-1beta and IL-6 in MAS development might be limited
- In addition, plasma exchange and high-flow continuous veno-venous hemofiltration have shown promise. The use of extracorporeal cytokine removal therapies (CytoSorb) may show some selective efficacy in such patients with MAS.
That was a great summary, I would also advocate for treating the underlying cause!
This concludes our episode on acute macrophage activating syndrome We hope you found value in our short, case-based podcast. We welcome you to share your feedback, subscribe & place a review on our podcast! Please visit our website picudoconcall.org which showcases our episodes as well as our Doc on Call management cards. PICU Doc on Call is co-hosted by myself Dr. Pradip Kamat and Dr. Rahul Damania. Stay tuned for our next episode! Thank you!

I love your episodes .
concise and lots knowledge
Thank you all ❤
Dr.abdullah pediatric resident saudi Arabia 🇸🇦
Good and elaborative podcast.
It will definitely help in patients care.
Thank you.