Welcome to PICU Doc On Call, A Podcast Dedicated to Current and Aspiring Intensivists.
I’m Pradip Kamat and I’m Rahul Damania and we are coming to you from Children’s Healthcare of Atlanta – Emory University School of Medicine.
Welcome to our Episode of a 9 year old girl with worsening seizures in the setting of an electrolyte abnormality.
Here’s the case:
A 9 year old girl presents to the ED with increased frequency of seizures, dehydration and listlessness. She has h/o of global developmental delay, congenital hydrocephalous (with VP shunt in place with her last revision 3 years prior, and seizure d/o treated with Leviteracetam. She usually has one or two focal seizures per day but on day of admission she had multiple prolonged seizures which were also generalized tonic clonic in semiology. Per her caregiver, the patient usually eats by mouth and mother typically gives her 3 cups of water daily. There is no history of diarrhea but patient has had 2-3 bouts of non-bloody non-bilous emesis on day of presentation. Looking at her growth chart, the patient has also lost ~ 2KG of her weight in the last 3 months and has had poor follow up with her PCP. In the ED she has a hypovolemic shock picture as she is hypothermic, tachycardic, tachpneic, and hypotensive with appropriate saturations. Blood gas is notable for a mild metabolic acidosis. Patient receives abortive seizure rescue. A head CT showed no increased in hydrocephalus, no mass or hemorrhage and a shunt series confirms patency of her VP shunt. Most pertinently to this case, her serum sodium on her RFP was undetectable at a value of = >200mEQ/dL; this was confirmed by a repeat lab draw and POC value. Other notable findings included an elevated Cr for age, an elevated BUN and a microcytic anemia. Patient was given a NS bolus, had cultures drawn, was started on broad spectrum abx therapy, stabilized and sent to the PICU.
To summarize key elements from this case, this patient has:
- A history of GDD with epilepsy and shunted hydrocephalus.
- A stigmata of cachexia.
- And a presentation of hypovolemic shock secondary to decreased intake, increased loss, and potential underlying concern for sepsis.
- The most important element of this case is her extreme hypernatremia
- All of these factors in this case point to our topic of discussion today → the approach to hypovloemic hypernatremia 2/2 to dehydration.
- Let’s transition into some history and physical exam components of hypovolemic hypernatremia?
- Key history features in patients who present with Hypovolemic HyperNa include:
- Increased losses such as emesis
- Decreased intake, and in this setting potentially lack of access to free water
- Listlessness which could be related to cerebral hypoperfusion
- Increase in seizure frequency due to increased rapid depolarization of Na channels in the brain and fluid shifts
- And weight loss → all of these factors were seen in our case.
- Of note if this patient was a neonate considering a high-pitched cry in the setting of hyperNa & dehydration could be a subtle history finding.
- Are there some red-flag symptoms or physical exam components which you could highlight?
- Our patient is Non verbal and has global delay secondary to a remote neurological insult
- She may not have intact ability to communicate or vocalize thirst.
- Apart from her mucous membranes, dry cracked lips, decreased skin turgor that can be described as doughy, and prolonged capillary refill, I think it is important to highlight her hypotension – as BP is one of the last vital signs in pediatrics to be abnormal in intravascular volume depletion. To me, this really stratifies this patient into severe dehydration and potentially septic shock.
This is a great point — understanding % volume loss and its correlation to vital sign and PE anomalies is key. Remember a sensitive marker for dehydration in pediatrics is tachycardia and a late finding if you are primarily dealing with dehydration is hypotension. This indicates that counter-regulatory responses are unable to maintain adequate systemic vascular resistance (SVR) and that there is a significant loss of intravascular volume. In our patient, we also noticed her weight loss on presentation which not only brings up the concern for malnutrition but it also serves as an adjunct measure of dehydration. In fact, in a 2009 paper assessing dehydration in pediatrics it was noted that the gold standard for confirming the diagnosis of hypovolemia in children is comparison of body weight before and after rehydration.
- To continue with our case, the patients labs were consistent with:
- Severe Hypernatremia
- Elevated BUN and Cr which point to an AKI
- And interestingly mild anemia → this could be a nutritional aberrancy such as iron deficiency anemia or anemia of chronic disease in the setting of her complex underlying condition but it also brings up the concern for hypovolemic shock secondary to bleeding. Pertinently she had no signs of external or internal bleeding, but it is important to stratify this element as your resuscitation efforts — i.e. whether you would give crystalloid or colloid can be guided by this subtlety.
Correct, it is important to highlight that in the setting of dehydration Hct values would be increased. In a 2006 Study in Transfusion, Valeri and colleagues concluded that the Hct values in hypovolemic anemic patients are elevated because the plasma volume does not increase to achieve the normovolemic anemic state.
OK to summarize, we have:
- 9 year old with global developmental delay who has emesis, dehydration and a serum Na of 200 mEq/L. This brings to the topic of our discussion today namely hypernatremia in the PICU.
- Let’s start with a short multiple choice question: 15 year old with h/o diabetes insipidus presents with a serum Na of 175mEq/L. 4 months ago his serum Na was 140mEq/L. Currently patient is obtunded with decreased skin turgor, fever and a blood pressure of 140/80 mmHg. Patient has been stressed due to school work and been non compliant with his DDAVP resulting in polyuria for almost 5 days.
- Treatment goal for this patient is
a. Reduce serum sodium concentration to normal in first 12 hours
b. Reduce serum sodium concentration to normal in 24 hours
c. Reduce serum sodium concentration to 150 mEq/L in 24 hours
d. Reduce serum sodium concentration by 10 mEq/L in 24 hours
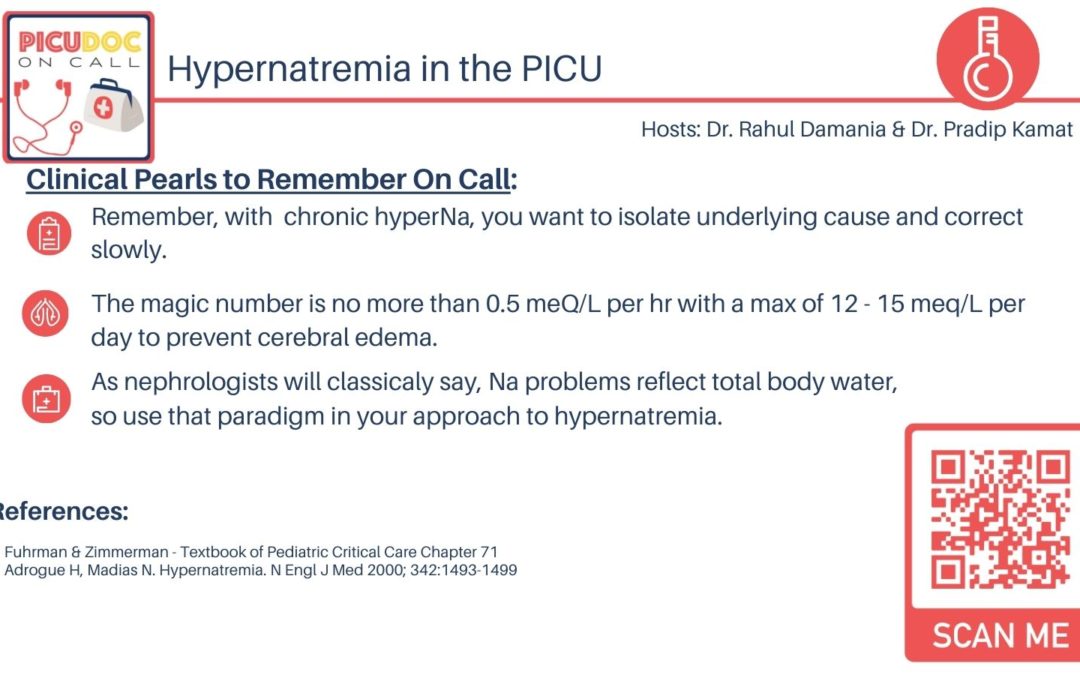
The correct answer is d. Reduce serum concentration by 10-12 mEq/L in first 24 hours; you can also think of this as not correcting the sodium more than 0.5 meQ/L per hour → thus in 24 hrs you should not lower the sodium by more than 12. I think listeners should remember that it is important to gradually lower the sodium in patients who have developed hypernatremia slowly over a period of days especially when Na is > 165mEq/L. Pradip, why is this?
- Patients with hypernatremia develop idiogenic osmoles to protect the brain from dehydration within hours. Numerous fatal cases of cerebral edema and herniation have occurred with rapid correction over a 24-hour period, leading to recommendations for correction over no less than 48 hours. General trend is for slow correction over 48 hours.
A mnemonic that can be useful is high to low the brain will blow; i.e. if a patient has chronic hypernatremia that is corrected too acutely, you have the potential to develop cerebral edema. In a landmark study published in NEJM in 2015, the authors concluded that rapid correction of hypernatremia can lead to cerebral edema to the relative inability of the brain to extrude idiogenic osmoles. Furthermore a study published in pediatric emergency care in 2013 showed that serum sodium correction rate > 0.5 mEq/L/hour was associated with increased risk of mortality and convulsion in neonates with hypernatremia dehydration admitted to neonatal intensive care unit.
Rahul: what would be some of the anatomic changes seen in the brain due to the resultant hyperosmolarity from hypernatremia?
- Anatomic changes seen with the hyperosmolar state include loss of volume of brain cells with resultant tearing of cerebral vessels due to local ECM shear stress forces. As you have an imbalance in frank starling capillary mechanics and subsequent flow through your cerebral vasculature, you may also see capillary and venous congestion, subcortical or subarachnoid bleeding, and interestingly, venous sinus thrombosis.
I’d like to make a big point about the phenomena of sinus venous thrombosis as this has been well described in Pediatric Review articles. Taking it back to the basics, Virchow’s triad gives us a framework on how to think about mechanisms of thrombosis. During hypernatremic dehydration at a micro-level there is endothelial stress and subsequent injury which can subsequently lead to venous sinus thrombosis. These patients can present with altered mental status, severe headache, and seizures.
Rahul, that was a great framework → as we conclude our podcast, Iets hone in on three areas: a schema in understanding hypernatremia, a diagnostic approach, and finally a management framework.
In general, how do you think about hypernatremia?
- I think Pradip one easy way to approach hypernatremia is to think of it as a water loss problem or a salt gain problem. Hypernatremia can exist as any of the following 3 scenarios, and these are all correlated to total body water.
- First, low total body water: Patients with a low total body water and hypernatremia have a loss of water in relative excess of sodium losses. This can occur from vomiting and diarrhea or renal losses from osmotic diuresis.
- Second Normal Total body Water: Loss of water occurs without excessive sodium losses in some conditions → these patients are going to be relatively euvolemic. Extrarenal losses result from increased respiratory losses as may occur with tachypnea, hyperventilation, or mechanical ventilation with inadequate humidification are examples of this phenomena.
- We also think about further insensible loss scenarios such as transcutaneous losses associated with fever, burns, extreme prematurity, or use of phototherapy or radiant warmers in the neonate without adequate water replacement. In general, another well-described cause of euvolemic hypernatremia is DI which can be a podcast in and of itself!
- Finally we think about increase in total body sodium and subsequent total body water: Usually from iatrogenic causes such as administration of Na HCO3, hypertonic saline or improperly concentrated infant formula.
- In a 2017 systematic review the authors looked at acute sodium toxicity due to dietary intake. They cited factors such as social media challenges and even charities that advocated eating small amount of salt to empathize with Syrian refugees. They concluded that a lethal dose of <5 teaspoons of salt ingested acutely can lead to pediatric fatality.
- If you had to work up this patient with hypernatremia what would be your diagnostic approach?
- I would highly suggest getting a nephrology consult in this patient.
- A comprehensive metabolic panel, Urine analysis
- Urine analysis especially of the first urine specimen preferably prior to rehydration to determine specific gravity
- If you are suspecting DI, getting urine Na and electrolytes may be indicated
- In this our patient case, she presented with increased seizures and altered sensorium, thus A CT scan of the head is recommended to evaluate for hemorrhage and shunt malfunction.
- Due to hypothermia a blood culture, urine CX, a CBC with diff, CRP and procal would be useful. As this child has concern for increased catabolism in the setting of failure to thrive and lack of access getting a CPK to rule out rhabdomyolysis as a cause of intrinsic AKI would be useful.
- Finally a renal US may be necessary based on laboratory and urinary findings.
I like this list Pradip, totally agree that a coordinated effort with nephrology can help in this setting as these patients may have renal dysfunction and there can be a collaborative effort in tracking electrolytes after we choose the appropriate rehydration fluid management. I would also recommend tracking weights as a part of your initial diagnostic plan!
- Our history physical and investigational undertaking has led us to severe hypernatremia as our diagnosis what would be your general management of framework?
- Patient needs to be adequately resuscitated to correct hypotension, protection of airway, and if necessary AEDs to control of seizures. Continuous EEG monitoring must be considered especially if patient is intubated. Most importantly, correction of underlying disease process giving rise to hypernatremia should be the goal. In our case it was dehydration due to lack of access to free water.
- Gradual correction of serum hypernatremia ~ 12-15 mEq/L/day. Frequent monitoring of serum Na(Q2 hr initially), as well as close eye on UOP
- As hypernatremia is toxic to the beta islet cells, their dysfunction can lead to associated hyperglycemia.
- Estimated deficits, ongoing maintenance requirements, and additional excessive losses must be accounted for in calculations of the amount of fluid replacement required. In general 2-2.5 times maintenance IVF fluids usually with NACl is necessary especially with severe dehydration.
- In a precise academic approach calculating the free water deficit may be helpful:
- The equation is:
- 0.6 x wt (kg) x [(current Na+/140) – 1] = this gives you liters of fluids:
- In acute dehydration you can take this fluid deficit and resusicate 50% of the volume you calculate over the first 12 hrs, and the remaining in the next 24 hrs could be a potential management strategy.
- If patient has central DI: Vasopressin, DDAVP along with replacement of UOP may be needed.
- In hypernatremic dehydration, the intracellular fluid moves into the extravascular space due to hypernatremia hence the patients dehydration may be underestimated.
- If patient has renal failure dialysis may be necessary