Welcome to PICU Doc On Call, A Podcast Dedicated to Current and Aspiring Intensivists.
I’m Pradip Kamat
and I’m Rahul Damania and we are coming to you from Children’s Healthcare of Atlanta – Emory University School of Medicine.
Welcome to our PICU Mini-Series Episode a 10 month old who is intubated for acute respiratory failure secondary to RSV bronchiolitis.
Here’s the case:
A 10-month-old full-term infant girl old is intubated for acute respiratory failure secondary to RSV bronchiolitis. Patient was brought to the ED by parents on day 3 of her illness with h/o cough, congestion and worsening respiratory distress. She has had increasing WOB and grunting. After assessment in the ED where the patient had a brief trial of HFNC, she was intubated with a 4.0 ETT due to persistent hypoxemia. Pertinently, her viral panel was positive for RSV, and the patient was transferred to the PICU. In the PICU, patient was ventilated using PRVC: Set TV of 90cc (patient is 11KG), PEEP 6, PS 10, and FIO2 40%. Throughout her course, she was mechanically ventilated and sedated for about a week. She required a continuous infusion of rocuronium due to decreased lung compliance and high peak pressures. Patient weaned on her ventilator settings by ICU day 7 and the decision to move towards extubation was made.
To summarize key elements from this case, this patient has:
- 10 month old with acute respiratory failure secondary to RSV infection and with a secondary bacterial infection due to H.Influenza.
- Had about a six day course on the ventilator requiring sedation and NMB
- and now we are at the discussion of extubation readiness.Rahul, do you mind summarizing the patient’s peri-extubation course?
Sure Pradip, so on day 6 of hospitalization our patient was weaned to low mechanical ventilator settings. The chest radiograph, which initially showed evidence of interstitial pneumonitis and atelectasis now improved and the patient had improved secretion burden. The patient was on ceftriaxone throughout the hospital course as her ETT cx with which grew Hemophilus Influenzae.
- What about the patient’s neurological status?
- The patient was initially on fentanyl, dexmedetomidine and a rocuronium infusion — a day prior to considering extubation, the patient was off of the continuous rocuronium infusion oxygenating and ventilating well. The patient prior to extubation was wide awake and appropriate during the morning sedation holiday.
- Any other important clinical markers?
- Yes, the patient’s clinical exam including lung exam was reassuring. The patient underwent a pressure support trial PEEP 5, CPAP 10 and had a normal respiratory effort with exhaled of about 5 mL/kg. The RT, however mentioned that the patient did not have a “leak” when performing the leak test. The finally the patient was given a few doses of furosemide for diuresis prior to extubation.
- Awesome, today’s episode we really want to focus on extubation readiness however prior to this discussion, can we take a step back and talk about some red-flag symptoms which led to intubation for this patient?
- This patient had severe respiratory distress which progressed to failure.
- The tachypnea, decreased mentation, and grunting were key signs that the patient was progressing to endotracheal intubation.
- Grunting is important to highlight as this refers to the child generating auto-PEEP to combat the atelectasis present in bronchiolitis.
- Remember that a child’s chest wall has a high compliance and a decreased propensity for outward elastic recoil — this in essence reduces FRC and thus there is a more balance towards the inward recoil of the long (closing capacity). The highly compliant chest wall and the natural inward recoil of the infant lung creates a propensity towards atelectasis and subsequent impairments in breathing. Low FRC can also create increase PVR which can thus imbalance optimal cardiopulmonary interactions.
OK let’s transition to our topic of discussion by a quick summary:
- A 10 month old after 6 days of MV is now ready for extubation.
- Let’s start with a short multiple choice question:
- In children deemed ready for extubation by clinicians, which of the following is most likely to be associated with reintubation?
- A) High breath by breath variability
- B) Failed Pressure Support trial
- C) Duration of mechanical ventilation
- D) No leak around the ETT prior to extubation
- Correct answer is A. Pediatric extubation failure rate ranges from 2-20%. Although extubation failure is usually multifactorial, High respiratory variability during spontaneous breathing trials is independently associated with extubation failure in children.
- A recent paper by Kelby et al in CCM 2020-found that after controlling for confounding variables such as age and neurologic diagnosis, reported that both coefficient of variation of respiratory rate and decreased maximal change in airway pressure generated during airway occlusion had almost 3-fold higher risk of extubation failure. When this subset of children developed post-extubation upper airway obstruction, reintubation rates were greater than 30%.
- What about the other factors we had in our answer choices like the Pressure Support Trial?
- Children fail PS trial for variety of reasons including ETT size, sedation, to name a few. Khemani and colleagues (Intensive Care Med. 2016 Aug; 42(8):1214-22)reported that regardless of endotracheal tube size, pressure support during extubation readiness tests significantly underestimates post-extubation effort of breathing.
- Further, A 2009 paper by Newth et al (Pediatr Crit Care Med. 2009 Jan;10(1):1-11.) reported in systematic review of weaning and extubation for pediatric patients on mechanical ventilation, that extubation failure bore little relationship to the duration of MV.
- I think it is important to highlight that though we frequently perform PS trials, we should assess other factors such as primary reason for extubation being reversed, secretions, and even neuromuscular components – extubation does not just refer to lungs being ready to have less support!
- Yes Rahul, absolutely agree — I do want to mention A controversial topic has always been the utility of measuring a leak pressure around the ETT to predict upper airway obstruction. A study by Khemani et al (Am J Respir Crit care 2016 Jan 15;193(2):198-209) reported the risk factors independently associated with subglottic UAO, included low cuff leak volume or high preextubation leak pressure, poor sedation, and preexisting UAO (P < 0.04) for cuffed ETTs; and age (range, 1 mo to 5 yr) for uncuffed ETTs (P < 0.04). For uncuffed ETTs, the presence or absence of preextubation leak was not associated with subglottic UAO.
- Lets summarize – upper airway obstruction involves checking if there is flow (in the form of pressure) surrounding the ETT — key point younger patients (1 mo to 5 yr old) with uncuffed tubes have risk to develop UAO peri-extubation.
- An older study by Wratney et al (Pediatr Crit Care Med. 2008 Sep;9(5):490-6) had previously reported that an endotracheal tube air leak pressure >/=30 cm H2O measured in the non-nparalyzed patient before extubation or for the duration of mechanical ventilation was common and did not predict an increased risk for extubation failure. The authors in that study concluded that- Pediatric patients who are clinically identified as candidates for an extubation trial but do not have an endotracheal tube air leak may successfully tolerate removal of the endotracheal tube.
- This suggests that having a leak may not be necessary for a patient to successfully extubate.
- So Rahul for our listeners What are factors associated with extubation failure?
- Thats an excellent question. Factors correlated with an increased risk of extubation failure include a longer duration of sedative use, younger age, higher complexity of medical conditions, and diaphragmatic dysfunction. The most common reported cause of extubation failure in pediatric patients is upper-airway obstruction, with other causes that include respiratory insufficiency, muscular weakness, cardiac dysfunction, and neurologic impairment. Duration of MV, PRISM III score did not predict extubation in a multivariable analysis reported by Krasinkiewicz et al (Respiratory Care April 2021 Vol 66 No 4).
Pradip, What are the main barriers to extubation in pediatrics?
Thats an excellent question Rahul. One study published in Respiratory Care in` 2021 Vol 66 No 4) reported that in patients who had their passed the extubation readiness test, most common reason for holding off extubation was a planned procedure, neurologic diagnosis/status of the patient, and no leak around the ETT, other factors included high ventilator rates and over sedation, hemodynamic instability, fluid status etc.
I think it is important for us to truly consider procedures or imaging which are planned to play a factor in our timeline for extubation readiness – this mitigates the risk for re-intubation – which is especially important in children with difficult airways!
Rahul: how do majority of children’s hospitals perform extubation readiness test prior to extubation?
- I think Pradip there is considerable variation in the methodology of ERT. Some common practices which I have noted as a fellow include: A daily spontaneous breathing trial performed probably early in the am (~4am) by the RTs. As long as patient didn’t require any procedure (imaging or surgery), hemodynamically stable, patient spontaneously breathing, FIO2 < 50% (some use 40%), PEEP ≤ 6cm H2O, SPO2 > 92% and TV exhaled ~ 6-8cc/kg on PIP ≤25 cm H2O. These are the patients who we deem on minimal vent settings. The sedation is decreased or a propofol bridge is added followed by a switch to PS CPAP trial (PS 8-10cm H2O and CPAP of 5cm H2O) for at least 2 hours. It is also important to correlate PO status with timing of extubation especially if the patient does well with the SBT.
- After switching to PS/CPAP If patient has no hemodynamic issues, hypoxia, increased WOB and a normal blood gas, the patient’s secretions are manageable, upper air reflexes are intact and neuromuscular function is sufficiently good to achieve an adequate vital capacity and maximum inspiratory pressure, GCS > 8—patient is considered a likely candidate for extubation. Most institutions will also check a leak around the ETT the night before. Some may decide to use a dose of decadron prior to extubation (although this is not supported by pediatric studies). Some extubate patient directly to room air, whereas others may use NIPPV such as CPAP or HFNC.
- Pradip, what are the signs of failure of ERT and what should be done in patients who fail their spontaneous breathing trial?
- Rahul, Signs of failure during ERT: include apnea, Exhaled TV < 5ml/kg, tachypnea for age, increased respiratory effort, desaturation below target SpO2 and unstable hemodynamics. Patients SBT can be repeated later in the day, sedation, fluid balance etc may require modification of optimization. The concept of sprinting -where the patient is subjected to SBT and allowed to remain on PS/CPAP for few hours everyday and which is subsequently increased is useful in those who are slow to wean off their ventilatory support.
In essence this may optimize their neuromuscular strength.
- Can you comment on any objective indices used in pediatrics as predictors of successful extubation?
- Rahul two indices used to objectively predict success of extubation were the rapid shallow breathing index (RSBI) and the compliance, resistance, oxygenation, and pressure index (CROP index).
- A paper by Thiagarajan et al (Am J Respir Crit Care Med. 1999 Nov; 160(5 Pt 1):1562-6.) reported on 227 mechanically ventilated children.
- Extubation failures had higher RSBIs and lower CROP index values. A RSBI value of </= 8 breaths/ml/kg had a sensitivity of 74% and specificity of 74%, whereas a CROP value of >/= 0.15 ml/kg/breaths/min had a sensitivity of 83% and specificity of 53% for extubation success. IN contrast adult studies have shown that a CROP ≥ 13.5 ml/breat/min had a specificity of 91.9% and sensitivity of 87.9% in predicting extubation success.
- OK to summarize – high rapid shallow breathing index and poor compliance, resistance, oxygenation indices indicate negative predictors for successful extubation
Thats correct — for more detail, The RSBI is a ratio of spontaneous TV to RR (adjusted for age). the CROP index is the compliance, respiratory rate, oxygenation and pressure index. The CROP index (ml/ kg/breaths/min) was calculated using the formula: Cdyn × NIF × (PaO2 /PAO2 )/RR.
- Let’s break this down:
- Cdyn – is a function of plateau – peep / TV.
- NIF measures conducting zone resistance
- and the OI index involves patient gas as well as alveolar gas which brings into the FiO2 the patient is receiving.
Rahul what is the role of respiratory muscle weakness in extubation outcomes?
- Khemani et al (Crit Care Med. 2017 Aug; 45(8):e798-e805.) used respiratory measurements using esophageal manometry and respiratory inductance plethysmography to assess respiratory muscle strength and predict respiratory extubation failure.
- The authors reported in their study that 35% of children had diminished respiratory muscle strength (aPiMax ≤ 30 cm H2O) at the time of extubation, and were nearly three times more likely to be reintubated than those with preserved strength (aPiMax > 30 cm H2O; 14% vs 5.5%; p = 0.006). aPiMax = maximum airway pressure during airway occlusion (aPiMax). the authors concluded that Neuromuscular weakness at the time of extubation was common in children and was independently associated with reintubation, particularly when post-extubation effort was high.
To summarize Neuromuscular status is essential to assess peri extubation – this is especially true in patients with myopathies either stress, paralytic or steroid related or primary muscular dystrophies.
Correct, also, More recently Glau et al (Pediatr Crit Care Med. 2020 Sep;21(9):e672-e678) reported Diaphragm atrophy is associated with prolonged post extubation noninvasive positive pressure ventilation in children with acute respiratory failure.Serial bedside diaphragm ultrasound may identify children at risk for prolonged noninvasive positive pressure ventilation use after extubation. However There was no difference in diaphragmatic parameters (atrophy rate, and peri-extubation diaphragmatic thickness in expiration and inspiration) in extubation success versus failure (Mistri S. et al. Pediatr Pulmonol. 2020 Dec;55(12):3457-3464).
So Rahul to look at our case again, what about her metabolic alkalosis prior to extubation ?
- I generally correct metabolic alkalosis (when Sr HCO3 ≥30) using acetazolamide or chloride in form of K chloride. I also optimize Mag, Phos and Ca in any patient prior to extubation. I also optimize the nurtitional status with help of our PICU dietician as soon as a patient is intubated.
- To wrap up, Rahul, why should we extubate patients early?
Great question: There is increased morbidity from prolonged mechanical ventilation: To name a few— VAP, pneumothorax, muscle weakness, atrophy of diaphragm, pressure sores, subglottic stenosis (can happen in less than a week of MV), unplanned extubation with cardiac arrest, and prolonged ICU length of stay. Additionally delirium and need for abstinence medications and rehabilitation.
The SCCM’s ICU liberation ABCDEF bundle recommends use of spontaneous breathing trials and spontaneous awakening trials to improve patients outcomes. PCCM providers should strive for early mobility, minimal sedation, focus on analgesia as well as push to liberate patient from MV as soon as safely possible.
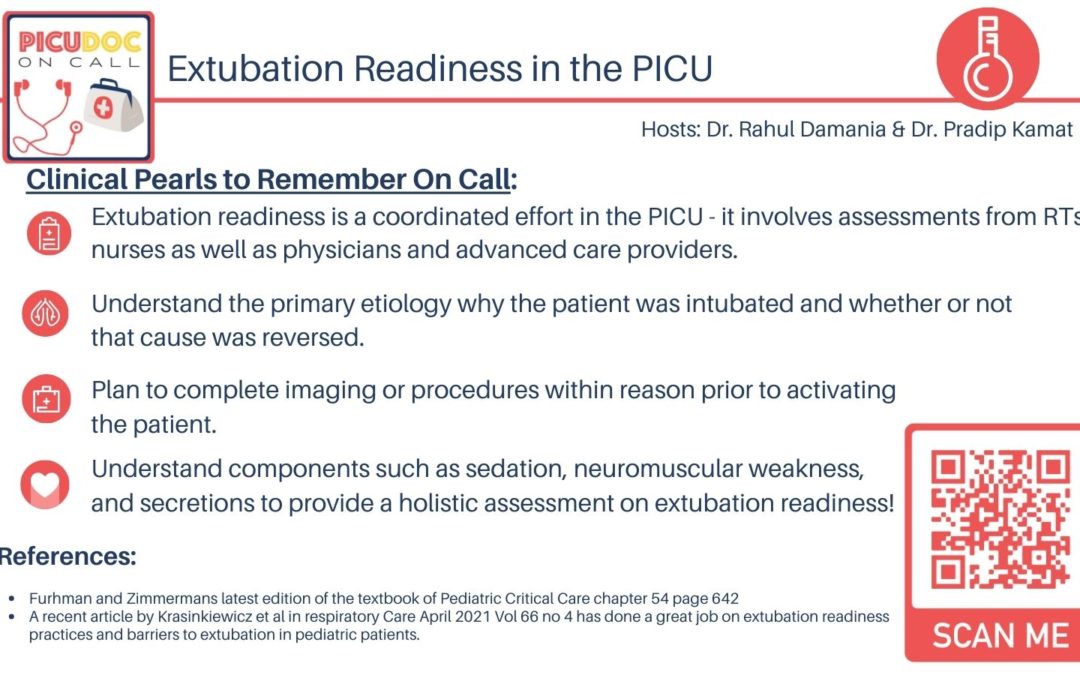
To highlight a key concept from today – extubation readiness is a coordinated effort in the PICU – it involves asessments from RTs nurses and as well as physicians and advanced care providers. Understand the primary etiology why the patient was intubated and whether or not that cause was reversed. Plan to complete imaging Or procedures within reason prior to activating the patient. Understand components such as sedation, neuromuscular weakness, and secretions to provide a holistic assessment on extubation readiness!
- Pradip – Are there any recent publications related to extubation success?
- Furhman and Zimmermans latest edition of the textbook of Pediatric Critical Care chapter 54 page 642
- A recent article by Krasinkiewicz et al in respiratory Care April 2021 Vol 66 no 4 has done a great job on extubation readiness practices and barriers to extubation in pediatric patients.
This concludes our episode on Extubation Readiness We hope you found value in our short, case-based podcast. We welcome you to share your feedback, subscribe & place a review on our podcast! Please visit our website picudoconcall.org which showcases our episodes as well as our Doc on Call management cards. PICU Doc on Call is co-hosted by myself Dr. Rahul Damania and my cohost Dr Pradip Kamat. Stay tuned for our next episode! Thank you!

Great podcast episode – but it’s actually about thyroid storm not extubation readiness. Perhaps just needs a quick fix.
Hello,
Great episode, but it’s about thyroid storm and not extubation readiness.
I am very interested about hearing your episode about extubation readiness.
Thank you.