Today’s episode focuses on salicylate toxicity, specifically in the case of a teenager with abdominal pain and emesis. Join us in this discussion of symptoms, patient history, diagnosis, management, and treatment.
Show Highlights:
- Our case: A 15-year-old female is admitted to the PICU for intentionally ingesting a large amount of aspirin tablets. She had epigastric abdominal pain with some non-biliary, non-bloody emesis when she presented to the outside emergency department twelve hours post-ingestion. She denies any neurological symptoms, including tinnitus but appears anxious and tachypneic. In the emergency department, her salicylate level was 45 mg/dL after her ingestion of about 250 aspirin tablets of 325 mg each. The patient is previously healthy, denies the use of illicit drugs and alcohol, is not sexually active, and has no allergies.
- To summarize the key elements of this case and patient history, she has ingested potentially toxic amounts of aspirin and has suicidal ideation but has no tinnitus or other neurological symptoms.
- Physical examination results show stable vital signs except for a temp of 38.8C; she has persistent tachypnea and mild epigastric tenderness but no rashes or previous cutting scars.
- Patient labs were consistent with a 12-hour salicylate level of 45 mg/dL, liver function, Bun/Creatinine, and coagulation profile are all normal. Her anion gap is slightly elevated, urine pH is 6, specific gravity is normal, and urine pregnancy test is negative.
- Based on patient history, physical exam, and labs, it appears that the patient has GI symptoms of early salicylate toxicity. Ingesting potentially toxic amounts of aspirin brings concern for life-threatening injuries to organs and possible loss of life. Let’s quiz ourselves with a short multiple-choice question:
- A teenager with a previous history of suicidal attempt now presents with confusion, increased respiratory rate, fever, and diaphoresis. Her physical exam including the pupillary exam is normal. Her labs are remarkable for a pH of 7.45, CO2 of 19, HCO3 of 11, serum anion gap of 20meQ/L, serum K of 2.9, and serum glucose of 180 mg/dL. There are weakly positive ketones in the urine. The next step in management of this patient is:
- A) NaHCO3 infusion
- B) Insulin infusion
- C) Oral activated charcoal
- D) Hemodialysis dialysis
- The correct answer to this question is A) Sodium bicarbonate infusion.
- Insulin therapy is not the answer because serum glucose is low, and a patient with a pH>7.25 is unlikely to have DKA.
- While activated charcoal can be used, especially followed by sorbitol given with the first dose, we need to be cautious about its use with an altered mental status as in the patient above.
- Since we do not have a salicylate level at this stage, offering hemodialysis should not be the first step, although it can be considered later given the neurological symptoms.
- Remember: Any patient with a previous history of suicidal ideation who presents with confusion, fever, and diaphoresis with the above labs is suggestive of mixed respiratory alkalosis with high anion gap metabolic acidosis is highly suggestive of aspirin poisoning. Always examine the pupils in any case of poisoning, as that may point one towards a possible toxidrome.
- Let’s highlight how basic science correlates with ASA poisoning:
- Remember the mechanism of action. Aspirin is a cyclo-oxygenase inhibitor which blocks prostaglandin production and has an antithrombotic effect by inhibiting platelet generation of thromboxane A2.
- Salicylates are weak acids which interfere with the Krebs cycle and specifically uncouple oxidative phosphorylation. This leads to acidosis, heat production, and hypoglycemia.
- Although not common, neuromuscular irritability manifested as paratonia (inability to relax muscles) and extreme muscle rigidity can develop, further contributing to hyperthermia and increasing the risk of rhabdomyolysis.
- Salicylates induce fatty acid metabolism resulting in ketone production which can further compound the anion gap metabolic acidosis.
- Disruption of the electron transport chain causes a dissociative shock picture in which there is adequate oxygen delivery, however, the tissues are unable to uptake the oxygen.
- Considerations in the diagnostic approach to our patient with salicylate poisoning:
- Salicylate poisoning can happen acutely (usually in young adults with suicidal ideation) or chronically, which often happens in the elderly who are taking aspirin therapeutically but have an inadvertent overdose. Because the pathways for salicylate elimination are fully saturated in those taking the drug chronically, a higher toxicity can occur at even a lower dose.
- The plasma level of salicylate required to elicit symptoms tends to be lower in chronic than in acute salicylate poisoning. In cases of acute salicylate toxicity, rising plasma levels are roughly correlated with the development of expected clinical manifestations, but such correlations are notoriously absent with chronic toxicity.
- Salicylate poisoning should be suspected in any patient with the following:
- Possible ingestion of known or unknown drug
- Tinnitus, nausea, vomiting, tachypnea, and altered mental status
- Elevated anion gap metabolic acidosis; remember that the patient can present with a mixed respiratory alkalosis and an anion gap metabolic acidosis
- Any elderly patient on chronic aspirin therapy who presents with agitation, confusion, hallucinations, slurred speech, seizures, and coma; “salicylate jag” refers to restlessness and mental aberrations that resemble alcohol intoxication
- Your diagnosis will likely be confirmed by elevated serum salicylate concentration!
- It is important to check salicylate levels with serial measurements every three hours because toxicity can be delayed. Once you get the level, you can stratify the level of toxicity:
- Generally, a level of 15-30 mg/dL is considered therapeutic for inflammatory conditions, but levels can exceed 40-50 within 1-2 hours of a single ingestion.
- Significant toxicity begins to manifest at a level >45 with tinnitus, vertigo, nausea, vomiting, and hyperventilation.
- A level of 50-70 indicates severe intoxication; the patient can have fever, sweating, listlessness, and incoordination.
- At levels exceeding 75, patients are at risk for hallucinations, seizures, cerebral edema, coma, noncardiogenic pulmonary edema, and cardiovascular collapse.
- Other major testing to consider include acetaminophen level, acid-base status with electrolytes, blood gas, urine pH, and pregnancy test, renal and liver function tests, and possible head CT if there are signs of cerebral edema or persistent altered mental status.
- If the history, physical exam, and diagnostic investigation lead us to a salicylate poisoning diagnosis, the general management framework would be as follows:
- Management is based on supportive care and elimination of salicylate, including gastric decontamination with activated charcoal and possibly polyethylene glycol via a nasogastric tube.
- The airway should be protected with intubation for respiratory failure, in the obtunded or delirious patient, or for a procedure such as dialysis access catheter placement. Avoid a low respiratory rate because any decrease in pH from a rising PCO2 can enhance movement of salicylate into tissues, and the patient can worsen.
- In fluid management, use Lactated Ringer’s solution since normal saline can cause normal anion gap acidosis and lower pH. A hallmark of therapy for salicylate ingestion is the alkalinization of the patient’s urine until the serum salicylate level is <40 mg/dL, metabolic acidosis is resolved, and the patient is asymptomatic with a normal respiratory rate. It is recommended to give one meQ/Kg initial bolus of NaHCO3 followed by three ampules of NaHCO3 added to one liter of D5W, with the goal of keeping the urine pH above 7.5. Add some KCL to this as hypokalemia can occur. Check serial blood gases, along with ionized calcium and magnesium, and avoid a serum pH above 7.5.
- Hemodialysis should be considered for the patient because the water solubility, small size, low volume of distribution, and absence of tissue binding make salicylate an ideal substance to dialyze.
- Urinary alkalinization is NOT a substitute for dialysis and can be stopped once dialysis is initiated.
- Hemodialysis should be considered for any patient with severe signs or symptoms, including severe fluid and electrolyte disturbances, altered mental status, cerebral edema, acute respiratory distress syndrome, and acute kidney injury.
- Hemodialysis is recommended if the plasma salicylate level is greater than 90 mg/dL or greater than 80 if kidney function is impaired.
- Conventional hemodialysis is preferred, but hemoperfusion or CVVH is acceptable if hemodialysis is not available or the patient is unstable.
- Keep close communication with poison control and the clinical toxicologist because of the life-threatening complications that can occur.
- Repeat the salicylate level at least every three hours until the level is down-trending.
- Learn more about salicylate toxicity from these sources:
- The review of salicylate toxicity by Palmer and Clegg from the New England Journal of Medicine, June 2020
- Chapter 126, p. 1503 of the latest edition of Fuhrmanns and Zimmerman’s textbook of Pediatric Critical Care
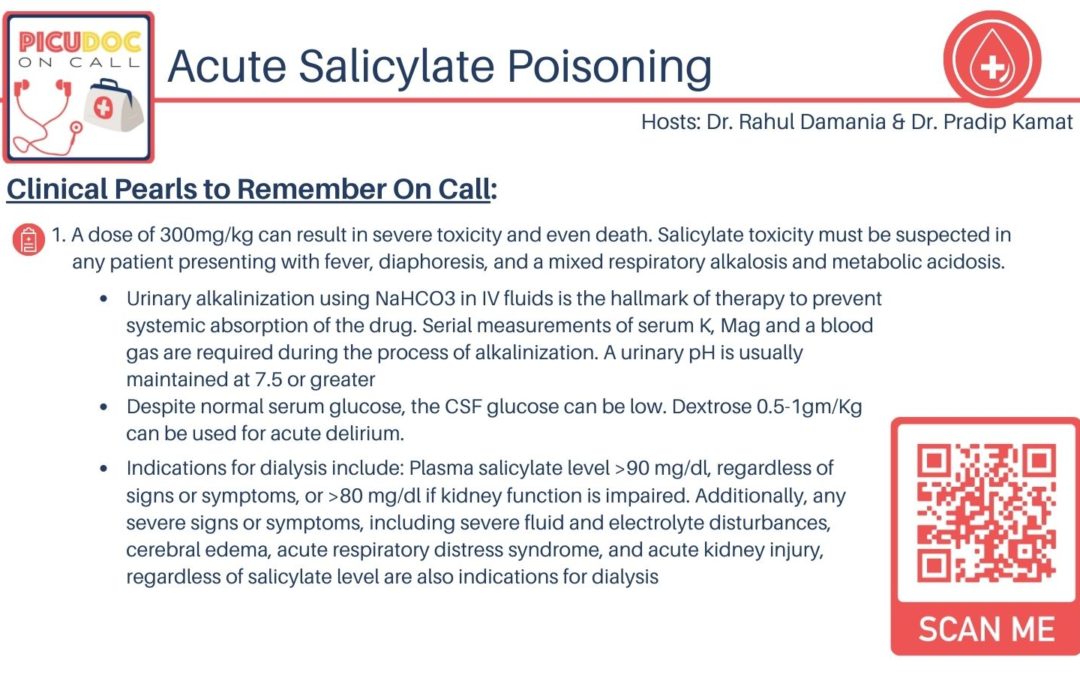
- Clinical pearls:
- A salicylate level of 300 mg/kg can result in severe toxicity and even death. Salicylate toxicity must be suspected in any patient presenting with fever, diaphoresis, mixed respiratory alkalosis, and metabolic acidosis.
- Urinary alkalinization using NaHCO3 in IV fluids is the hallmark of therapy to prevent systemic absorption of the drug. Serial measurements of serum K, Magnesium, and a blood gas are required during the process of alkalinization, and urinary pH should be maintained at 7.5 or greater.
- Despite normal serum glucose, the CSF glucose can be low. Dextrose can be used for acute delirium.
- Indications for dialysis include plasma salicylate level >90 mg/dL or >80 mg/dL if kidney function is impaired. Any severe signs or symptoms, including severe fluid and electrolyte disturbances, cerebral edema, acute respiratory distress syndrome, and acute kidney injury are indications for dialysis.