Today’s episode is dedicated to the intubation of the critically ill pediatric patient. Join us as we discuss the patient case, symptoms, and treatment.
We are delighted to be joined by Dr. Heather Viamonte. Dr. Viamonte is an Assistant Professor of Pediatrics at Emory University School of Medicine. She is a Pediatric Cardiac Intensivist at the Children’s Heart Center and the Director of Cardiac ECMO. The Children’s Heart Center is a 30-bed, dedicated cardiac intensive care unit at the Children’s Healthcare of Atlanta at Egleston. She is a newly published author whose book, Wilde Type, has already been released, and a second novel is on its way to publication. Dr. Viamonte is on Twitter as @hk_jacobs.
Show Highlights:
- Our case, symptoms, and diagnosis: A four-month-old patient is admitted to the PICU from the emergency department for acute respiratory failure on high-flow nasal cannula. The child’s condition has slowly deteriorated over the last few hours and now requires intubation. An echo is performed pre-intubation due to enlarged cardiac silhouette on chest radiograph demonstrating left ventricular dysfunction with ejection fraction in the low 40s. The patient’s saturations are dipping to the mid-80s despite being on maximal HFNC support.
- Common indications for intubation in the PICU or CICU include acute respiratory failure, upper airway obstruction, hemodynamic instability, management of increased ICP, mediastinal masses, protection of the airway, as well as for procedures and safe transport.
- Patient conditions with a high risk prior to endotracheal intubation include congenital or acquired heart disease, an infant or child with hemodynamic instability, pulmonary hypertension, upper airway obstruction, increased ICP, and mediastinal masses.
- Factors in infants and children with congenital heart disease that make them high risk for intubation include anatomical or physiologic issues that could lead to cardiac arrests, such as systemic ventricular dysfunction, single ventricle physiology, arrhythmias, pulmonary hypertension, and coronary artery anomalies.
- Why an understanding of the patient’s past medical history and overall physiology are important for risk stratification
- Anatomical concerns that should be assessed in infants and children prior to intubation include genetic syndrome heart defects that could interfere with bag-mask ventilation, airway visualization, or laryngoscopy. These could include morbid obesity and abnormalities of the face, mouth, and teeth.
- In conceptualizing congenital heart defects prior to intubation, the overriding concern is blood flow to the heart and lungs. Three factors to consider are volume overload, pressure overload, and systemic hypoxemia.
- Patients can have anatomical and physiological difficulties with regards to airway management, especially in those who are critically ill and those with cardiac disease.
- Four important clinical scenarios for physiologic derangements are hypoxemia, hypotension, metabolic acidosis, and congenital heart lesion pathophysiology.
- Remember that infants and children have a higher fragility factor and are at a higher risk for rapid desaturation, hypoxic brain injury, and cardiac arrest.
- Key factors for the intensivist are fine attention to detail, optimizing your monitoring equipment, and anticipating risk factors for peri-intubation cardiac arrest.
- Special considerations with intubation for the patient with severe metabolic acidosis are necessary to prevent cardiovascular collapse and pulmonary hypertension.
- How systolic dysfunction from either ventricle plays into the process of intubation
- Factors to consider to mitigate risk in intubation include preparation, a multidisciplinary approach, intubation equipment nearby, and management of the post-intubation period.
- Dr. Viamonte shares her perspectives on sedation and other medications to consider with intubation.
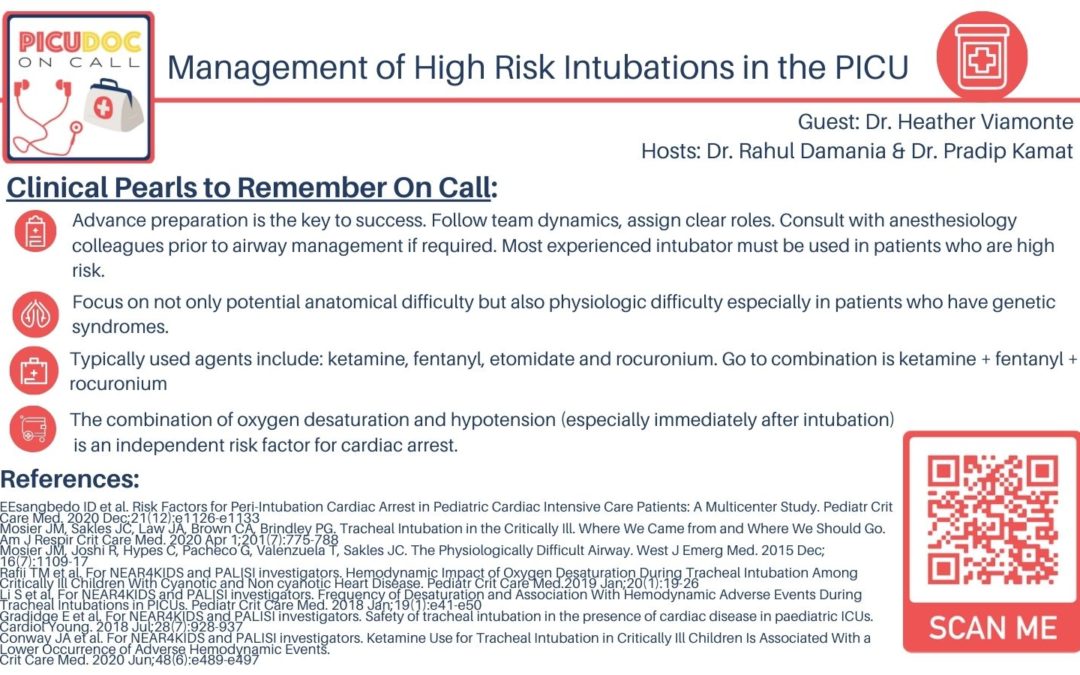
- Takeaway clinical pearls regarding intubation of the critically-ill, high-risk patient include maintaining the patient’s cardiopulmonary reserve, leveraging team potential and resources, and mitigating chaos. “Advance preparation is the key to success.”