Today’s episode is dedicated to the acute management of anterior mediastinal mass in the PICU. Join us as we discuss the patient case, symptoms, and treatment. We are delighted to be joined by Dr. Lisa Lima and Dr. Tom Austin.
Dr. Tom Austin is the Director of General Pediatric Anesthesiology at Children’s Healthcare of Atlanta-Egleston. He is also an Associate Professor of Anesthesiology and Pediatrics at Emory University School of Medicine.
Dr. Lisa Lima is a Fourth Year Advanced Technology Fellow in the Division of Critical Care at Children’s Healthcare of Atlanta. She’s also the Senior Associate in the Department of Pediatrics at Emory University School of Medicine. She’s one of the only pediatric-trained ECMO Fellows in the country.
Show Highlights:
- Our case, symptoms, and diagnosis: A 17-year-old female has facial swelling and shortness of breath. She recently went to her primary care physician and received a steroid burst and Benadryl for the facial swelling. On the day of admission, her mother noticed that the patient had a deep voice and a “funny” inspiratory sound. The patient presented to the ER and was noted to have a widened mediastinum on a chest x-ray, bringing up concern for an anterior mediastinal mass.
- Key presentation features for mediastinal masses
- What defines a widened mediastinum?
- Important differentials to consider with mediastinal masses:
- Take the patient’s history and presentation into context, like if there was a high-impact motor vehicle collision, history of congestive heart failure, lupus, transplant, leukemia, or lymphoma
- Pay attention to the Four T’s: thymoma, teratoma, ATLL(lymphoma), and thyroid masses
- Key principles that might put pediatric patients with mediastinal masses at risk for anesthetic agents
- Important pathophysiologic issues for patients with mediastinal mass include compressed trachea, blocked access to lungs, and right ventricular failure; these effects can be magnified under general anesthesia
- Why we need to have great appreciation of the risk of cardiovascular collapse in patients in a tenuous physiological state
- General management strategies for those patients who are unable to lie flat or may not tolerate a diagnostic scan: patient history, personal physical exam, determining a rescue position
- Key considerations for the patient in the PICU:
- Keep the patient spontaneously breathing
- Have adequate access with large-bore IVs in sites with no anatomic compression
- Have a rescue position
- Have a backup plan for rapid deterioration
- Communicate with others on the patient care team
- Why the Chamberlain procedure is used to obtain a tissue biopsy when there isn’t another primary biopsy site
- Key anesthesia principles for patients needing intrathoracic biopsies:
- Have clear role assignments in the multidisciplinary team approach
- Keep the patient spontaneously breathing
- Manage the patient’s pain
- Employ liberal use of local anesthetics
- Avoid intubation if possible
- If necessary, use fiber optic intubation
- Keep large-bore IVs in extremities
- Why it’s important to stress interdisciplinary involvement early in management
- Key factors to consider in patients headed to the OR about airway compression and vascular compression
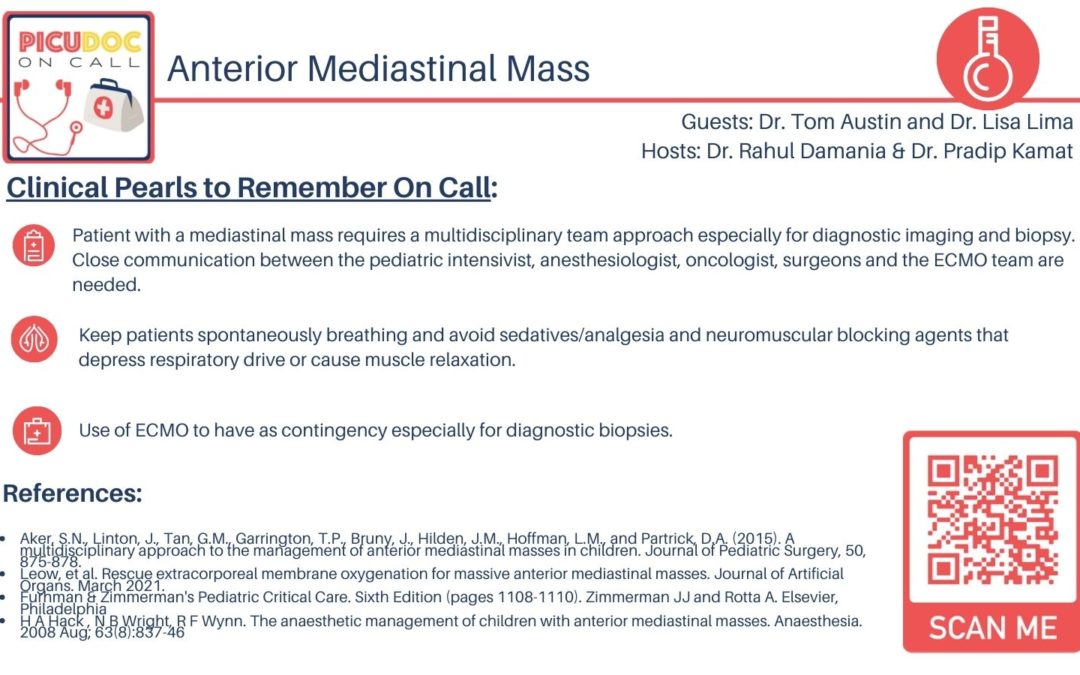
- Takeaway clinical pearls regarding anterior mediastinal masses:
- Remember the Four T’s
- The pathophysiology of local compression
- Emphasize a streamlined multidisciplinary approach with important considerations for contingency planning