Today’s episode is dedicated to acute management of laryngospasm. Join us as we discuss the patient case, symptoms, and treatment.
Joining us is Dr. Tom Austin, director of General Pediatric Anesthesiology at Children’s Healthcare of Atlanta-Egleston. He’s also an associate professor of anesthesia and pediatrics at Emory University School of Medicine.
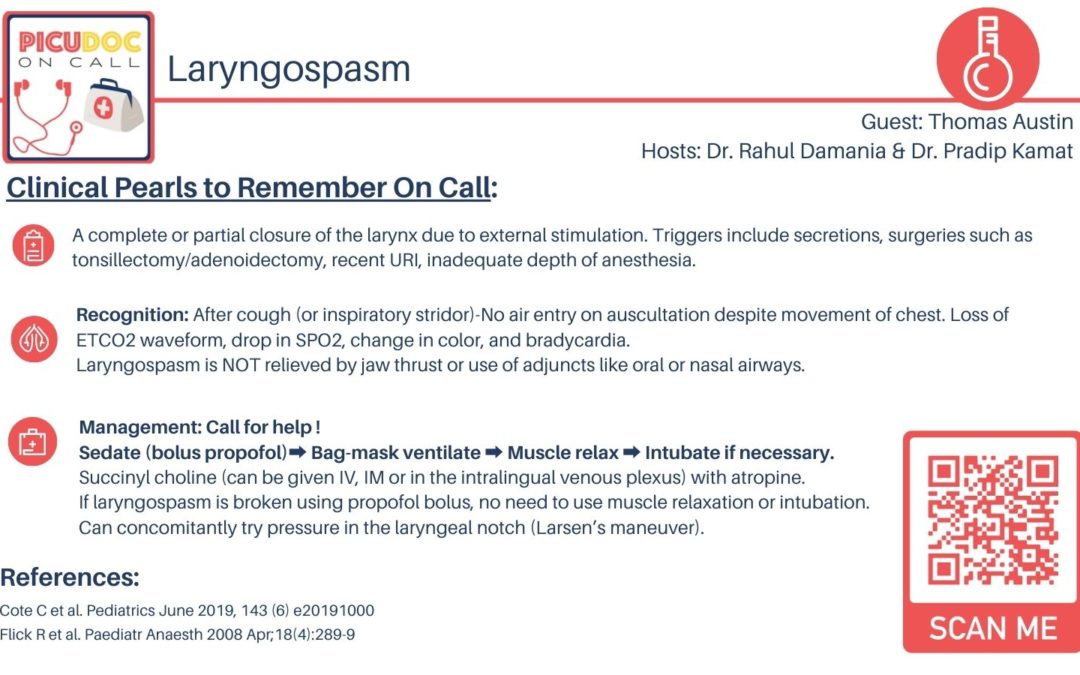
>>Click here to download the PICU card for this episode<<
Show Highlights:
- Our case: a two-year-old male with a history of Wilms’ tumor presents in a sedation suite for post-surveillance MRI
- History, symptoms, and treatment: One-week history of nasal congestion with no active nasal discharge and clear lung sounds. Patient was placed on continuous pulse ox symmetry and CO2 monitoring. With sedation for the MRI, the patient had a sudden cough, which progressed to perioral cyanosis and loss of end-tidal CO2.
- How this case illustrates laryngospasm
- Definition of laryngospasm: complete or partial closure of the larynx due to some manner of external stimulation
- Why laryngospasm leads to acute respiratory failure in children
- How laryngospasm differs from airway obstruction
- Characteristic breathing pattern with laryngospasm
- Acute management of laryngospasm includes a bag-mask and positive pressure ventilation, followed by deepened sedation, and a breathing tube
- Why early recognition of laryngospasm is the key