Today’s episode is dedicated to the acute management of pediatric stroke. Join us as we discuss the patient case, symptoms, and treatment.
Joining us is Dr. Elissa Ortolani, Assistant Professor of Pediatrics in the Division of Child Neurology and Assistant Professor of Neurology at Emory University School of Medicine. Dr. Ortolani has a strong clinical interest in pediatric vascular disease and is one of the few pediatric neurologists who has completed a formal adult stroke fellowship. She is actively helping to develop a pediatric stroke program at Children’s Healthcare of Atlanta.
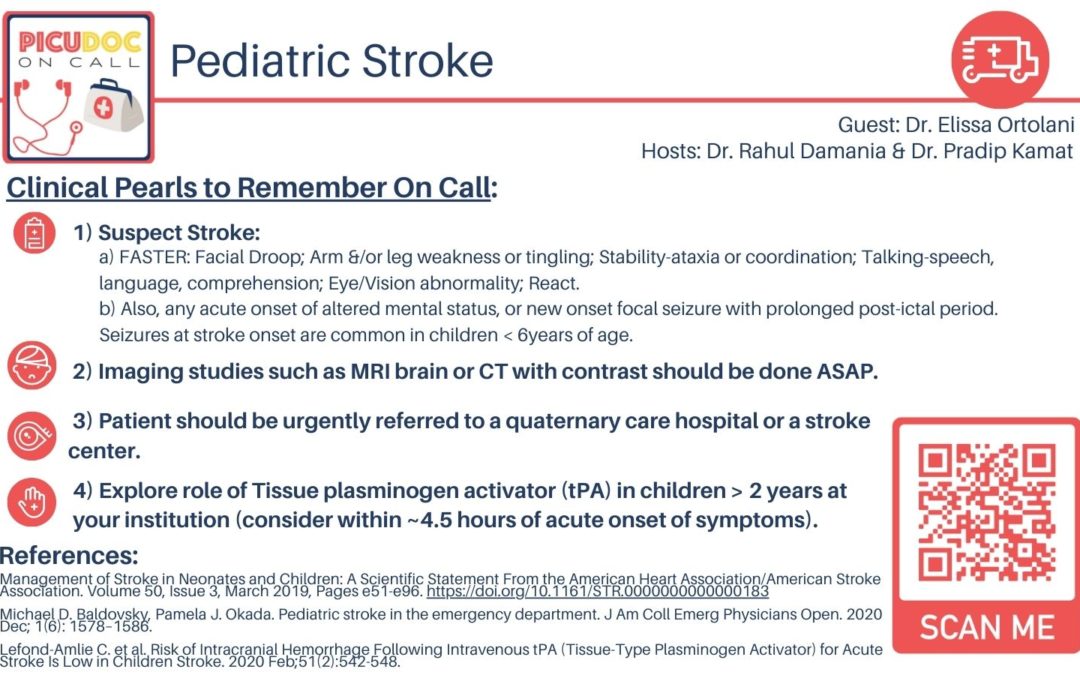
>>Click here to download the PICU card for this episode<<
Show Highlights:
- Our case: a five-year-old male, previously healthy, has had cold symptoms for two days; he presents to the ER with possible stroke symptoms
- Symptoms: the patient has had left arm and left leg weakness during the past day, and his mother noticed a subtle left side lip droop with drooling
- Acute management: In the ER, a CT revealed a subtle hypodensity in the right basal ganglia region; the patient was admitted to PICU for further monitoring and workup
- Causes of an acute pediatric vascular event can include stroke, seizure, migraine, and toxidrome
- Definition of stroke: an acute neurologic change identified by advanced imaging
- Practical tools in evaluating stroke include F-facial droop, A-arm weakness, S-speech difficulty, T-time. (Now, amended to FASTER to include stability and eyes/vision)
- Risk factors for pediatric stroke include vascular issues like sickle cell disease, congenital heart problems, thrombophilia, and mitochondrial, inflammatory, or connective tissue disease
- In pinpointing pediatric stroke or stroke mimic, which is very common, MRI is the preferred imaging method
- Important considerations in the diagnosis of pediatric stroke are that mild sedation is sufficient for the 10-12 minutes needed for MRI
- In the management of pediatric stroke, TPA should be administered within 4.5 hours, and endovascular therapy (if needed) should be administered within 24 hours
- Why the diagnosis and management of pediatric stroke is delayed, and how ER and ICU physicians can change that
- Developing a pediatric stroke program is a collaborative effort among emergency care providers, radiologists, pharmacists, adult neuro interventionalists, ICU team, neurosurgeons, hematologists, and rehab physicians
- A key in the diagnosis of pediatric stroke is recognizing altered mental status