Today’s episode is dedicated to post-operative management of liver transplant patients in PICU. Join us as we discuss the patient case, symptoms, and treatment.
Joining us is Dr. Joe Magliocca, Associate Professor of Surgery in the Department of Surgery at Emory University School of Medicine. He is also the Surgical Director of Adult and Pediatric Liver Transplantation at Children’s Healthcare of Atlanta.
Also joining the conversation is Dr. Rene Romero, Professor of Pediatrics at Emory University School of Medicine and Medical Director of the Liver Transplant Program at Children’s Healthcare of Atlanta, which is one of the largest liver transplant programs in the country with over 600 pediatric liver transplants to date.
>>Click here to download the PICU card for this episode<<
Show Highlights:
- Our patient, symptoms, and treatment: An 18-month-old with a history of biliary atresia is admitted to PICU after an orthotopic whole liver transplant. The patient is intubated, and Doppler ultrasound shows vascular patency post-operatively. AST and ALT are pending.
- Common indications for pediatric liver transplantation:
- 500-700 pediatric liver transplants are performed annually in the US
- 40% of the transplants are done on children born with biliary atresia
- 10-15% of the transplants are due to acute liver failure
- 5% of the transplants are due to malignancies
- The rest of the transplants are due to different childhood diseases and metabolic diseases
- How the PELD (Pediatric End-Stage Liver Disease in children under 12) score relates to prioritization for liver transplant
- Criteria for the PELD score are bilirubin, albumin, age, growth parameters, and INR
- The major differences between whole organ vs. split liver transplantation (long-term outcomes are similar and good for both situations)
- Why liver transplantation requires less immunosuppression than other organ transplants
- Three phases of the liver transplant process are the hepatectomy phase, anhepatic phase, and reperfusion phase
- Specifics of the time intervals during the transplant process, where the major risk is for primary non-function during cold ischemia and warm ischemia times
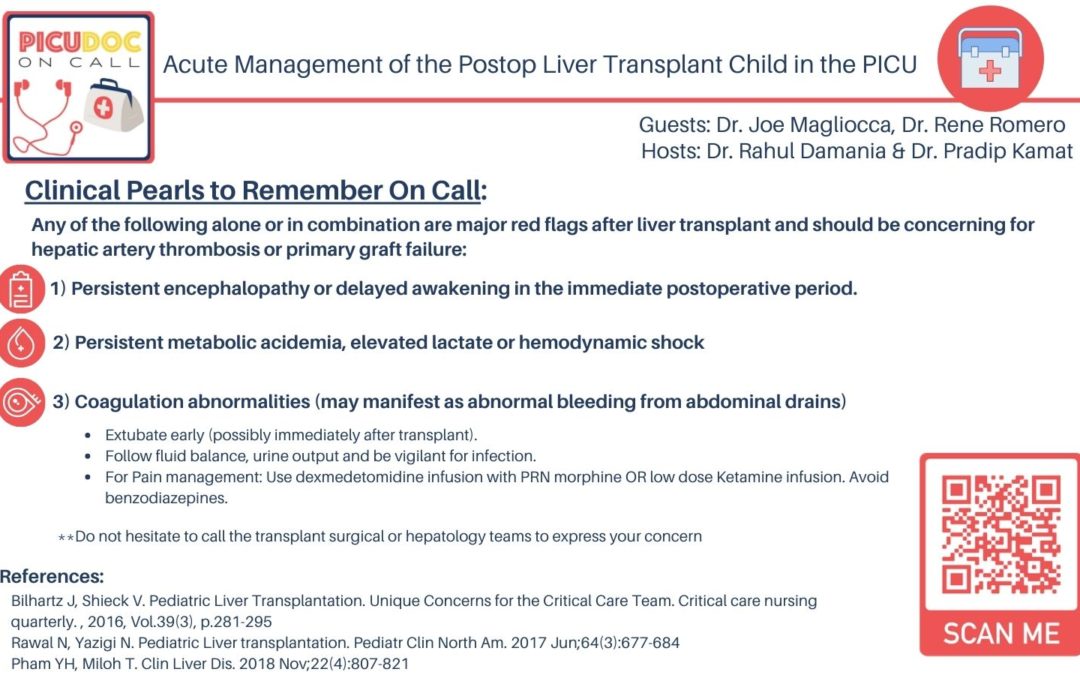
- Major red flags to look for during the immediate post-operative period
- Acute post-op management includes extubation in the OR, CV monitoring, pain management, checking urine and electrolyte levels, and communication with the transplant surgeon and liver team
- How treatment and management have evolved over time with standardized post-op management, protocols, and parameters
- Two important aspects of post-op management are nutrition and immunosuppression
- Clinical pearls of wisdom:
- The need for organ donors is great.
- Teamwork and collaboration are essential for good patient outcomes.
- The transformation in the field of liver transplantation has saved many children’s lives.