Today’s episode is dedicated to pediatric acute liver failure. Join us as we discuss the patient case, symptoms, and treatment.
Joining the conversation is Dr. Rene Romero, Professor of Pediatrics at Emory University School of Medicine and the Medical Director of the Liver Transplant Program at Children’s Healthcare of Atlanta.
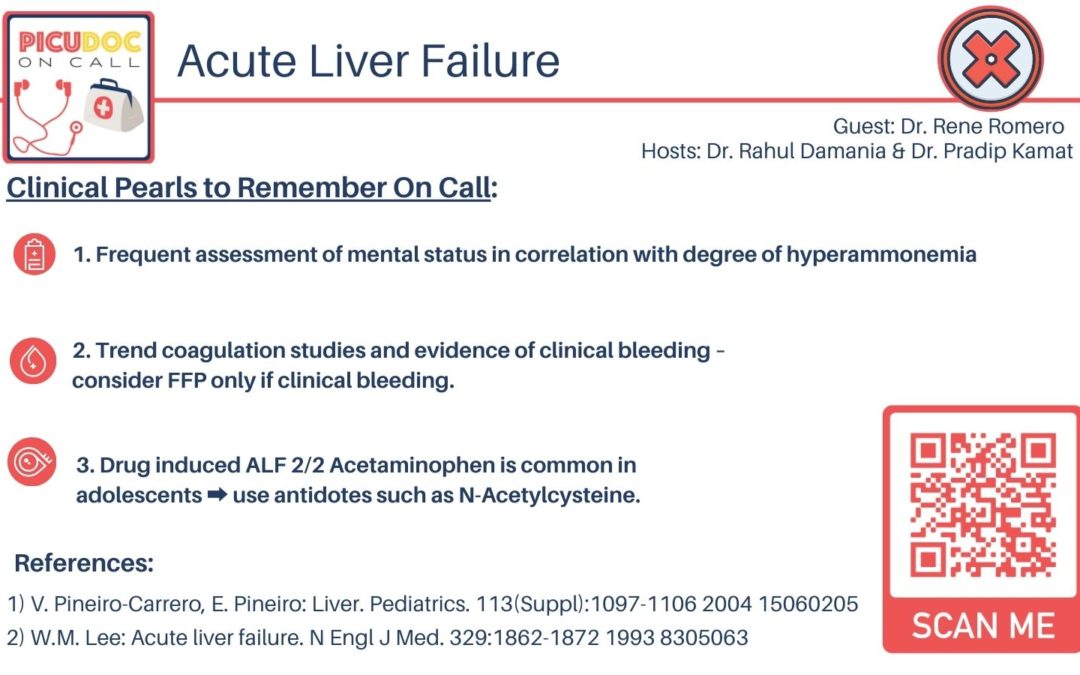
>>Click here to download the PICU card for this episode<<
Show Highlights:
- Our case, symptoms, and diagnosis: a three-year-old child presents in the PICU with decreased arousal; the patient is hypoglycemic. The coagulation panel is significant for increased PTT and INR, and AST and ALT are significantly elevated. The patient is hyperammonemic, and the acetaminophen level is normal. The diagnosis is acute liver failure.
- Basic functions of the liver, the “workhorse of the body” that plays major roles in interactions with other organs
- Why pediatric acute liver failure is more difficult to diagnose than in adults; key indicators are coagulopathy along with biochemical disruptions
- The most important contributing factors to pediatric acute liver failure, and why most pediatric cases are children under four years of age
- Causes of pediatric acute liver failure in the US include HSV, adenovirus, enterovirus, metabolic causes, and acetaminophen, especially in older children
- The diagnostic approach considers infectious etiologies, toxins, vascular issues, and immune dysregulation
- In treatment, care should be given to the correction of abnormal lab values and possible renal replacement therapy
- Why the use of prophylactic antifungal antibiotics is controversial and varies from institution to institution
- How to discern hyperammonemia and neurologic status
- The role of intracranial pressure monitoring for cerebral edema, which is the mode of death for these patients
- Key Clinical Pearls: acute liver failure is a systemic disease that requires a broad diagnostic approach, and the need for standardized approaches still exists.