Today’s episode is dedicated to acute metabolic emergencies. Join us as we discuss the patient case, symptoms, and treatment.
Joining us is Dr. Lori-Anne Schillaci, trained in clinical pediatric genetics with additional training in metabolism. She had a dual appointment in the Department of Pediatric Emergency Medicine at Rainbow Babies and Children’s Hospital, as well as an appointment in the Department of Genetics and Metabolism. Dr. Schillaci is currently embarking on a fellowship in Pediatric Emergency Medicine at Wake Forest Brenner Children’s Hospital.
>>Click here to download the PICU card for this episode<<
Show Highlights:
- Our case: A three-month-old infant presents with seizures and decreased oral intake
- History, symptoms, and treatment: The child is hypothermic and tachypneic. Blood gas is notable for anion-gap metabolic acidosis. Blood cultures are drawn, and antibiotics are started. Urine organic acids and serum ammonia are both pending.
- A metabolic emergency is defined as a defect in the breakdown or storage of the body’s energy sources (sugar, fat, and protein) at the cellular level
- Why metabolic conditions can be inherited or result from a spontaneous mutation
- How the toxic products form in the body and can affect children in three categories (protein, fat, and sugar metabolism)
- Common lab tests would be for ammonia, gas, and blood sugar
- Why the physician should save a purple top tube before any transfusion
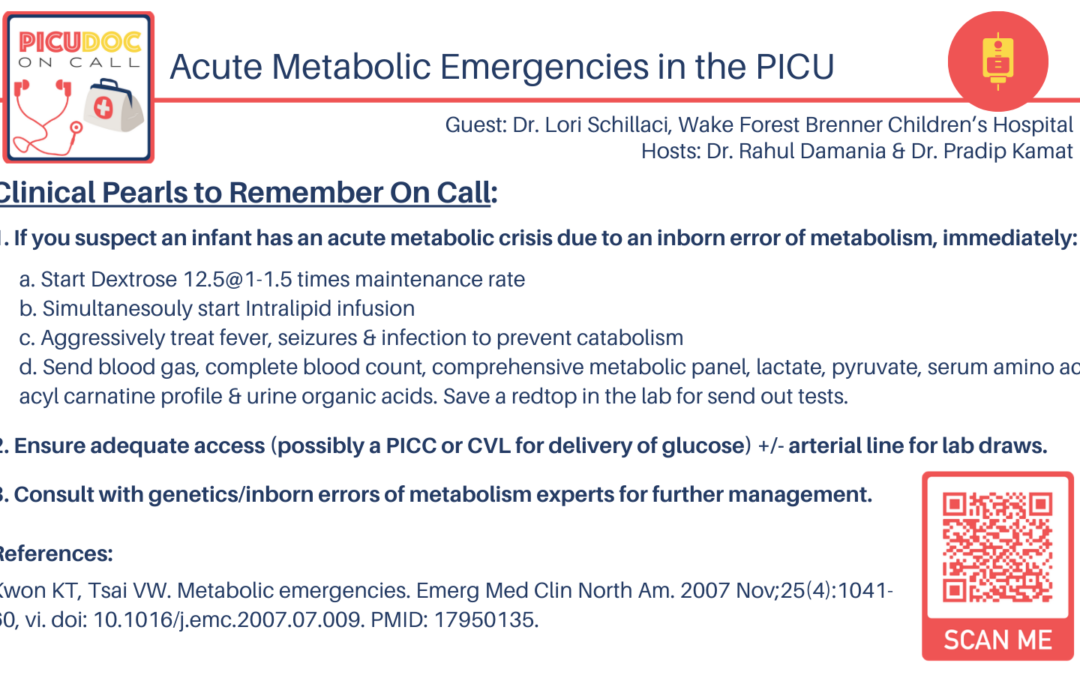
- General management should include treatment of the underlying acute issues, early dextrose fluids, normal saline fluid boluses, IV lipid emulsion (except in patients with known fatty acid oxidation defects)
- Advice to colleagues in managing a patient with inborn error:
- Keep in mind that the presentation can occur in older kids
- Get early labs when they are sick
- Start high dextrose fluids
- Keep the patient NPO
- Treat fever, hypoglycemia, seizures, infection, etc.
- The goal is to prevent catabolism and be aggressive early in treatment
- Dr. Schillaci’s final thoughts: “Be vigilant. Assume an inborn error of metabolism unless proven otherwise. Be aware of late presentations of inborn errors of metabolism.”